Jwara
Jwara (different types of fever)
Jwara is an important disease. The term ‘Jwara’ implies the ability of a disease to cause anguish to body and mind. [SAT-C.7][1] This suggests suffering or illness. Based on the similarity in clinical features, Jwara is often considered as fever or pyrexia in medical terminologies. However, according to Ayurveda, the classical description of jwara includes variety of other clinical conditions with or without rise in body temperature. Therefore, fever or hyperpyrexia is considered as only one among the many features of jwara.
| Section/Chapter/topic | Chikitsa / Jwara |
|---|---|
| Authors | Deole Y.S.1, Aneesh E.G.2 |
| Reviewed and edited by | Basisht G.3 |
| Affiliations |
1Department of Kayachikitsa, G.J.Patel Institute of Ayurvedic Studies and Research, New Vallabhvidya Nagar, Anand, Gujarat, India 2Charak Samhita Research, Training and Development Centre, I.T.& R.A., Jamnagar,India 3Rheumatologist, Orlando, Florida, U.S.A. |
| Correspondence emails: | dryogeshdeole@gmail.com, carakasamhita@gmail.com |
| Date of first publication: | February 15, 2022 |
| DOI | 10.47468/CSNE.2022.e01.s09.088 |
| Publisher | Charak Samhita Research, Training and Development Centre, I.T.R.A., Jamnagar, India |
Jwara is the commonest clinical condition observed in medical practice either as a primary disease or as a secondary sign owing to other morbidities. Hence it is given prime importance among all diseases. [Cha.Sa. Sutra Sthana 25/40] Calor (rise in temperature), rubor (redness), dolor(pain), tumor (swelling) are the cardinal signs of inflammation. Pathogenesis of jwara includes change in body temperature, discoloration, aches. Therefore, jwara is also an indicator of inflammatory changes in body.
As per conventional medical literature, the word fever has its etymological basis in Latin, meaning simply ‘heat’, and pyrexia comes from the Greek ‘pyr’, meaning fire or fever. It is caused by pyrogenic and non-pyrogenic conditions. Micro-organisms like bacteria, viruses etc. cause infection and body temperature is raised as an immune response to fight infection. Inflammatory chemicals like prostaglandins, cytokines play key role in pathophysiology of fever.[2]
Considering conventional literature on fever and ayurvedic perspective of jwara, similarities about involvement of thermoregulatory mechanisms are observed in etiopathogenesis and clinical features. However, the treatment measures are different. The conventional measures focus on reducing body temperature and removing the origin of infection using anti-biotic medicines. Ayurveda medical literature emphasizes on strengthening the host immune response or defense mechanism, correcting the equilibrium of body components and preservation of health.
This article describes general etiology, premonitory features, clinical features, pathogenesis, and management principles of jwara. Classification of the disease is also highlighted. Specific types of jwara like acute stage (nava jwara), chronic stage (jeerna jwara), irregular pattern (vishama jwara), jwara involving all three dosha (sannipataja jwara), jwara affecting body components (dhatugata jwara) are dealt in separate articles.
Diagnostic codes
- National Ayurveda Morbidity Code: EC -3
- ICD code for relevant condition/DSM code: R50.9 (ICD)
Keywords: Jwara, fever, roga, rise in body temperature, hyperpyrexia, infectious disease, noninfectious diseases in Ayurveda.
Jwara
Causes
- Dietary: Unwholesome food habits, taking meals during indigestion, irregular dietary habits
- Lifestyle: Excessive physical activities, exercise, fatigue, not following the seasonal regimens (ritucharya)
- Psychological: Sudden change in emotional status, grief, excess indulgence in any activity
- Others: Sudden change in season or abnormal climatic conditions, improper or excessive administration of purificatory procedures, trauma, degenerative conditions, infectious diseases, suppurations, exposure to poisonous gases, toxins; improper management of pregnancy, prenatal and postnatal care, abnormal changes in spiritual, lunar, planetary and constellation cosmic energies (nakshatra peeda)[Su.Sa.Uttara Sthana. 39/19-22][3]
Classification
I. Based on origin: 1. Endogenous (nija) and 2. exogenous (agantu)
1. Endogenous
- Vata dosha dominant
- Pitta dosha dominant
- Kapha dosha dominant
- Vata pitta dosha dominant
- Pitta kapha dosha dominant
- Vata kapha dosha dominant
- Vata pitta kapha dosha dominant [Cha.Sa.Nidana Sthana 1/17]
2. Exogenous [Cha.Sa.Chikitsa Sthana 3/111]
- Owing to injury (abhihataja)
- Owing to emotions like fear, anger (abhishangaja)
- Owing to wrong rituals and religious practices (abhicharaja)
- Owing to curse or negative energies (abhishapaja)
II. Based on the severity of symptoms
- Mild/low grade due to dominance of soma (saumya)
- High grade or severe due to dominance of agni (agneya) [Cha.Sa.Nidana Sthana.1/32]
III. Based on site of origin
- Physical or somatic
- Mental or psychic [Cha.Sa.Chikitsa Sthana 3/32]
IV. Based on the site of manifestation:
- Internal feeling (antarvegi)
- External features (bahirvegi) [Cha.Sa.Chikitsa Sthana 3/33]
V. Based on the time of manifestation
- Seasonal
- Unseasonal [Cha.Sa.Chikitsa Sthana 3/33]
VI. Based on the prognosis 1. Curable 2. Incurable [Cha.Sa.Chikitsa Sthana 3/33]
VII. Based on frequency of episodes [Cha.Sa.Chikitsa Sthana 3/34]
It is of 5 types.
- Continuously present (santata)
- Episode once in 24 hours (satata)
- Episode twice in 24 hours (anyedyushka)
- Episodes on every third day (tritiyaka)
- Episodes on every fourth day (chaturthaka)
VIII. Based on affected body tissues (dhatugatajwara)
- Nutritional fluid (rasa)
- Blood (rakta)
- Muscle (mamsa)
- Adipose tissue (meda dhatu)
- Bone (asthi dhatu)
- Bone marrow (majja dhatu)
- Semen/reproductive fluid (shukra)[Cha.Sa.Chikitsa Sthana.3/35]
Clinical features
Premonitory features
General premonitory features
Premonitory features of jwara include abnormal taste in the mouth, heaviness in the body, aversion to food, restless eyes, lacrimation, excessive sleep, restlessness, yawning, bending, shivering, exhaustion (without physical activity), giddiness, delirium, sometimes sleeplessness, horripilation, oversensitive teeth; tolerance and intolerance to sound, cold, wind and heat; anorexia, indigestion, weakness, body-ache, malaise, reduced vitality, mental agitation, lethargy, idleness, lack of natural activities, apathy to daily regimen, disrespect to the words of elders, agitation with children, aversion to doing work, uncomfortable with flowers and perfumes, aversion to sweet edibles, and desirous for sour, salty and pungent things. [Cha.Sa.Nidana Sthana 1/33]
| Jwara | Specific premonitory feature |
|---|---|
| Vata dosha | Excessive yawning |
| Pitta dosha | Burning in eyes |
| Kapha dosha | Dislike for food |
- [Su.Sa.Uttara sthana.39/27][3]
Exogenous fever (agantuja jwara) manifests directly without any prodromal symptoms. [Cha.Sa.Nidana Sthana 1/30]
General clinical features
Absence of perspiration, feeling of heat or raised body temperature and generalized body ache.[Su.Sa.Uttara Sthana 39/13][3] Discomfort in body and mind[Cha.Sa.Chikitsa Sthana 3/31], anorexia, morbid thirst and pain in cardiac region. [Cha.Sa.Chikitsa Sthana 3/26-27]
Features of manasajwara (mental origin): Mental instability (vaichitya), dislike for everything (arati) and feeling of weakness in the body (glani) [Cha.Sa.Chikitsa Sthana 3/36]
Features of internal feeling (antarvegi): Excessive burning sensation inside the body, morbid thirst, delirium, dyspnoea, giddiness, pain in bones and joints, absence of sweating, obstruction of dosha and feces.
Features of external manifestation (bahirvegi): Excessive rise in the body temperature and other features of internal feeling in mild form.
Seasonal manifestation: The seasonal changes cause dosha aggravation leading to kapha dominant jwara in spring (vasanta), pitta dominant jwara in autumn (sharada) and vata dominant jwara in rains (varsha). These are natural (prakrit) disequilibrium and do not need any treatment. [Cha.Sa.Chikitsa Sthana 3/42] [A.Hr Nidana Sthana.2/50][4]
Severe manifestation with deep affliction of body tissues (gambhiradhatugata): Sensation of internal heat, excess thirst, retention of faeces and flatus, severe dyspnoea and cough. [Su.Sa.Uttara Sthana.39/92][3]
Dosha specific clinical features
Vata dominant jwara
- Abrupt onset and remission
- Irregular pattern of rise in temperature and severity.
- Increase in post digestive phase and during times of vata aggravation like evening, early morning, and rains.
- Rough skin
- Greyish discoloration of nails, eyes, face, urine, stool and skin.
- Reduced urination and defecation
- Excessive tearing of nails, etc.
- Debilitating pain radiating from the toe to upper body, with various sensations felt at various parts as the pain travels – numbness in feet, cramps in the calves, looseness in knee joints (and also in all other joints), weakness in thighs, excruciating pain in the waist region, aching in the sides, pressure sensation in back, churning in shoulder, cutting sensation in arms and scapular region and constricting feeling in chest, inability to move the jaws, tinnitus, and piercing pain in the temple region.
- Astringent taste or lack of taste in the mouth (distaste), dryness of mouth, palate and throat; thirst, catching pain (grabbing pain) in the heart, dry vomiting, dry cough, loss of sneezing and eructation, aversion to the taste, salivation, anorexia, diminished digestive power, malaise, increased yawning, bending, shivering, exhaustion, giddiness, delirium, insomnia, horripilation, sensitivity in teeth, and the desire for hot things. [Cha.Sa.Nidana Sthana 1/21]
Pitta dominant jwara
- High intensity
- Increase during digestion of meals, midday, mid night or in the autumn season.
- Pungent taste in the mouth, ulceration or inflammation of the nose, mouth, throat, lips and palate, unquenchable thirst
- Narcosis, giddiness, fainting, vomiting of bile (pitta), diarrhea, aversion to food, malaise, dejection, delirium, appearance of reddish patches in the body, green or yellow coloration in nails, eyes, mouth, urine, faeces and skin, excessive migraine and burning sensation, desire for cold things.[Cha.Sa.Nidana Sthana 1/22-24]
Kapha dominant jwara
- Mild intensity
- Increase after taking meals, forenoon, early night or spring season.
- Heaviness in the body, less desire to eat, excess secretion of phlegm, sweet taste in the mouth, nausea, wrapped feeling in the heart, wheezing, vomiting, mild appetite, excessive sleep or narcolepsy, stiffness, drowsiness, cough, dyspnea, coryza, coldness, whiteness of nails, eyes, face, urine and skin, urticarial patches, desire of hot things and surroundings. [Cha.Sa.Nidana Sthana 1/27]
Vata pitta dominant jwara
- Desire of cold things [Cha.Sa.Chikitsa Sthana 3/37]
- Headache, breaking pain in joints, burning sensation, horripilation, dryness of throat and mouth, nausea, thirst, fainting, giddiness, anorexia, sleeplessness, talkativeness.[Cha.Sa.Chikitsa Sthana 3/85-86]
Vatakapha dominant jwara
- Desire of hot things [Cha.Sa.Chikitsa Sthana 3/37]
- Feeling of cold, heaviness, drowsiness, timidity, pain in joints, feeling of stiffness of head (shirograha), coryza, cough, impaired sweating and moderate rise in temperature. [Cha.Sa.Chikitsa Sthana 3/86-87]
Kapha Pitta dominant jwara
- Inconsistent sensation of hot and cold
- Frequent increased or decreased sweating, delusions, cough, anorexia, thirst, elimination of phlegm (kapha) and bile (pitta), coating and bitterness in the mouth and drowsiness. [Cha.Sa.Chikitsa Sthana 3/87-88]
Severe manifestation affecting ojas (hatojas jwara):
- Displacement of ojas due to aggravation of vata and pitta dosha
- Stiffness or rigors in the body, desire to sleep, loss of consciousness, drowsy, delirium, feeling of horripilation, mild rise in temperature associated with body ache. [Su.Sa.Uttara Sthana 39/43-44][3]
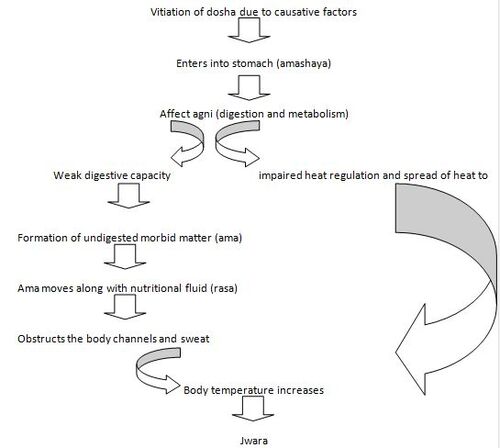
Pathogenesis
- Dosha: Pitta dominance associated with vata and kapha
- Dushya: Nutritive body fluids (Rasa dhatu)
- Agni: Jatharagni
- Srotasa: Channels of transportation of nutrient fluids and sweat (rasavaha, swedavaha)
- Site of origin: stomach (amashaya)
- Site of manifestation/clinical presentation: Whole body and mind [Cha.Sa.Chikitsa Sthana 3/30]
- Type of pathogenesis: Obstruction (sanga)[Cha.Sa.Chikitsa Sthana 3/ 129-132] [Su.Sa.Uttara Sthana.39/24][3] [A.Hr Nidana Sthana 2/3-5][4]
- In jwara due to trauma (abhighata), blood (rakta) is the vitiated primarily;
- In jwara due to negative energies (abhishangaja), vata and pitta are vitiated
- In jwara due to fascination (abhichara) and wrath (abhishapaja), all dosha are vitiated. [Cha.Sa.Nidana Sthana 1/30]
Biomarkers for diagnosis and assessment of efficacy
Clinical features are observed to diagnose the condition. Changes in body temperature are recorded.
For diagnosis:
- Body temperature above 36.5 – 37.5 degree celsius (97.7 – 99.5 degree fahrenheit)
- Rectal temperature: 37.5 – 38.3 degree celsius (99.5 – 100.9 degree fahrenheit) and above
- Oral temperature: 37.7 degree celsius (99.9 degree fahrenheit) and above
- Axillary temperature: 37.2 degree celsius (99.0 degree fahrenheit) and above
Investigations:
Complete blood count, Urine culture, Widal test, Mantoux test, PCR test, Viral culture, Sputum examination, Chest X-ray etc. These laboratory and radiological investigations are useful in finding causative microorganism and nature of infective agents. The investigations are done only in severe conditions of disease and weak patients.
Prognosis
Easily curable (sukhasadhya)
- External manifestation (bahirvegi) of jwara [Cha.Sa.Chikitsa Sthana 3/41]
- Seasonal manifestation [Cha.Sa.Chikitsa Sthana 3/42]
- Jwara in a person with good physical and mental strength, or if caused by the vitiation of lesser amount of dosha and without any complications. [Cha.Sa.Chikitsa Sthana 3/50]
Difficult to cure and poor prognosis
- Jwara caused by either greater amount of dosha/ strong etiological factors
- Jwara manifests with multiple clinical features
- Jwara which acutely affects the sense organs.[Cha.Sa.Chikitsa Sthana 3/51-52]
- Severe manifestation, associated with delirium, giddiness and breathlessness causes death of the patient
- Jwara in a weak and emaciated person (kshina), associated with edema (shuna), seated in deeper body tissues (gambhira), severe (balvan) and persistent for long durations (dirgharatrika) are incurable. [Cha.Sa.Chikitsa Sthana 3/52-53]
- Jwara due to psycho-spiritual factors like allure and wrath is incurable. [Cha.Sa.Nidana Sthana 1/30]
- Jwara caused by vata dosha is difficult to treat in any season. [Cha.Sa.Chikitsa Sthana 3/49] Pitta dominant jwara occurring in seasons other than autumn and kapha dominant jwara occurring in seasons other than spring are difficult to treat. [Cha.Sa.Chikitsa Sthana 3/49]
Management
Objectives of treatment or goals of treatment
The treatment of jwara is decided after assessment of sama (afflicted with ama) status of dosha. In case of afflicted with ama status, the treatment is to naturally promote digestive and metabolic processes. This changes the status of ama and pacifies afflicted dosha resulting in their normal functions.
In premonitory or preclinical stage
- Therapeutic fasting and measures to create lightness in body (langhana) is highly effective in early stages of jwara and prevents further progression. [Cha.Sa.Nidana Sthana 1/36]
- If the dosha are not afflicted with ama, then administration of cow ghee in vata dominant jwara, mild purgation in pitta dominant jwara and therapeutic emesis in kapha dominant jwara are prescribed on observation of premonitory features. [Su.Sa.Uttara Sthana 39/97-98][3]
Principles of management on observation of clinical stage
The principles of management of jwara include correcting disequilibrium of dosha and maintaining strength of the host simultaneously. Natural remission through sequential prescription of measures of fasting, fomentation, thin gruel consumption, use of medicines with bitter taste and those promoting digestion is emphasized. [A.Hr Chikitsa Sthana 1/21][4]
Fasting or lightening therapy (langhana) is the first line of treatment. It promotes digestion of toxins, produces lightness and alleviates raised body heat.[Su.Sa.Uttara Sthana.39/103][3]
Hydration is maintained by advising hot water consumption. Hot water stimulates digestion, disintegrates kapha and ama, helps in the normal functioning of vata and pitta, quenches thirst and produces lightness in body. It is helpful in dominance of kapha and vata dosha. [Su.Sa.Uttara Sthana.39/106-107][3]
These measures are intended to remove obstruction in channels, improve digestion and pacification of vitiated dosha to their normal state. [A.Hr Chikitsa Sthana 1/39][4]
Suitable dietary regimen for 10 days followed by medicated ghee is advised.[A.Hr Chikitsa Sthana 1/82][4] After improvement and correction of digestion, the diet to improve strength of individual such as meat soup, yusha etc. are advised.
After attaining proper strength, purification therapies to remove toxins and prevent recurrence are prescribed.
Precautions
Contraindications of fasting:
Fasting is contraindicated in jwara caused by aggravated vata dosha or by exertion or by traumatic or psychic causes, and in chronic conditions. [Cha.Sa.Chikitsa Sthana 3/272] [Su.Sa.Uttara Sthana.39/102][3]
Contraindications of hot water:
Hot water is contraindicated in conditions occurring due to pitta dosha, , burning sensation of eyes and whole body; delusion and diarrhoea, poisoning and alcoholic intoxication; in summer season, in emaciation and bleeding disorders.[A.Hr.Chikitsa Sthana.1/14][4]
If the strength of the individual is normal, then the medicines are administered at a suitable stage and only if required. The general period for natural remission is one week. If jwara does not subside and deterioration in condition is observed due to acute aggravation of pitta dosha, then medicines are prescribed. [Su.Sa.Uttara Sthana.39/119][3]
Consumption of ghee
- The disease jwara causes excess dryness and increased heat in the body. This further aggravates vata and pitta dosha. Ghee is administered to pacify vata and pitta dosha. It also nourishes dhatu and prevents depletion. [Su.Sa.Uttara Sthana.39/133][3]
Administration of milk
- In chronic stages, if the patient suffers from excessive burning sensation and thirst due to vata and pitta dosha, milk is advised.[Cha.Sa.Chikitsa Sthana 3/167-68]
Indications of pacifying therapy (shamana)
- If dosha is in less amount or if patient is emaciated, then dosha pacifying measures are advised instead of lightning measures. [Su.Sa.Uttara Sthana.39/134][3]
Indications for meat soup
- Meat soup is advised if digestive capacity is normal in emaciated and vata predominant conditions. [Su.Sa.Uttara Sthana.39/136][3] If the patient is not habituated to meat, then black gram soup is advised.
Medicinal herbs used in jwara: Tinospora cordifolia(guduchi), Zingiber officinale (nagara), Terminalia chebula (haritaki), Fumaria parviflora (parpata), Aconitum ferox (vatsanabha), Piper nigrum (maricha)
Herbal formulations: Amrutotaram decoction (kwatha) [5], Guduchyadi kwatha [B.R.5/156][6], Samshamani vati, Sudarshana churna [B.R.5/445-54][6], Amritarista [B.R.5/1257-60][6], Pathyadi kwatha
Herbo-mineral formulations: Jwaramurari rasa[B.R.5/881-887][6], Tribhuvanakeerti rasa [7], Anandabhairava rasa[B.R.6/161-63][6], Laxmivilasa rasa [B.R.5/1223-35][6]
Panchakarma procedures with safety precautions
Generally, panchakarma procedures are indicated when the dosha are free from affliction of ama state. [Su.Sa.Uttara Sthana.39/124-125][3]
- Fomentation (swedana): Different fomentation techniques are used judiciously in jwara patients. Mild fomentation by covering the body with thick blanket (guru pravarana) is indicated in initial stage. It clears obstruction in sweat channels and normalizes body temperature. If the patient is experiencing excess cold, rhinitis, dyspnoea, pain in calves, joints and bones, fomentation is indicated. After the elimination of dosha, if residual kapha and vata dosha are causing jwara, fomentation and massage is indicated.[Su.Sa.Uttara Sthana.39/319][3][A.Hr.Chikitsa Sthana 1/20][4]
- Therapeutic emesis (vamana): If kapha dosha is in excess aggravated state, emesis is administered. [Cha.Sa.Chikitsa Sthana 3/227][Su.Sa.Uttara Sthana.39/98][3] It is also indicated in the initial phase, conditions of nausea, excessive salivation, aversion to food, cough, simultaneous occurrence of vomiting and diarrhoea. It is ideal treatment if jwara manifests immediately after meals. [A.Hr.Chikitsa Sthana.1/5][4]
- Therapeutic purgation: It is prescribed in case of aggravated pitta dosha conditions. [Cha.Sa.Chikitsa Sthana 3/227] It should be performed only in later stage of jwara and if jwara does not respond to medicines; provided the patient is having good strength and digestive capacity. [Cha.Sa.Chikitsa Sthana 3/168-69] If dosha are free from ama state and retained in digestive tract (koshtha), purgative medication can be given even in acute stage of fever. [Su.Sa.Uttara Sthana.39/124][3]
- Medicated enema (basti): If the dosha are lodged in colon (pakwashaya) medicated enemas can be used.[Cha.Sa.Chikitsa Sthana 3/240]
- Intra nasal drug administration (nasya): Purificatory nasal medication is indicated for chronic conditions with heaviness, headache and impaired sensorium. [Cha.Sa.Chikitsa Sthana 1/173-74] If patient feels emptiness of head, have burning sensation, unctuous nasal medication which mitigates pitta should be administered. [A.Hr.Chikitsa Sthana.3/126][4]
- Bloodletting (raktamokshana): If the jwara is not responding to either cold or hot therapies or to unctuous or ununctuous therapies, bloodletting therapy should be performed. Here the dosha are located in the peripheral tissues, which can be eliminated only through bloodletting. [Cha.Sa.Chikitsa Sthana.3/289-90]
Wholesome diet and lifestyle factors
- Green gram (mudga), lentils (masoora), Bengal gram (chanaka), Trichosanthes cucumerina (patola), Momordica charantia (karavellaka), Moringa oleifera (shigru), Vitis vinifera (draksha), Punica granatum (dadima), hot water, gruel prepared from popped paddy etc. are wholesome in jwara conditions. Physical and mental rest, the seasonal regimen followed in summer is advised.
Unwholesome diet and lifestyle
- Diet items that are heavy to digest, unwholesome, mutually contradictory and cause burning sensation (vidahi) are contraindicated in jwara. Sexual intercourse, excessive physical activities, exhaustive works and head bath should be avoided. [Cha.Sa.Chikitsa Sthana 3/330-32]
Preventive aspects of recurrence
- If Jwara is not managed properly, it may recur due to residual dosha. Therefore, purification or pacification therapy should be done properly to prevent recurrence. A type of decoction enemas like ‘yapana basti’ and mild elimination therapies for the complete evacuation of dosha are advised to prevent recurrence. [Cha.Sa.Chikitsa Sthana 3/339]
Clinical features observed during remission of jwara
- During sudden remission, dosha undergo acute physiological transformation. Vomiting, increased respiration, profuse perspiration, tremors, delirium, altered state of consciousness are observed. The person expels foul smelling liquid feaces. [A.Hr. Nidana Sthana 2/76-78][4]
Clinical features after recovery
- Lightness of head and body, perspiration, slightly pale face with boils, sneezing, desire towards food; [Su.Sa.Uttara Sthana.39/318][3] absence of exhaustion and discomfort, ulceration in mouth, itching in head and normal functioning of sense organs are observed after recovery from jwara. [A.Hr. Nidana Sthana 2/79][4]
List of research works done
- Mathew Soosan (1983): Latakaranjabeeja ka Vishama Jvaramein kriyatmaka anvekshana, Department of Dravyaguna, IPGT&RA, Jamnagar.
- Dal D K (1981): Vishamajvara (malaria) chikitsatmaka adhyayana, Department of Kayachikitsa and Panchakarma, IPGT&RA, Jamnagar.
- Kishan T (1982): Effect of Bhoomyamalaki in Jvara (w.s.r to vishamajvara), Department of Kaumarabhritya, IPGT&RA, Jamnagar.
- Kashaih M (1983): A study on effect of certain indigenous drug in Vishamajvara, Department of Kaumarabhritya, IPGT&RA, Jamnagar.
- Sarvaiya D B (1987): Dravyavigyana of Bhramara-Challika and its therapeutic effect on Vishamajvara, Department of Dravyaguna, IPGT&RA, Jamnagar.
- Varsha Solanki (1998): A comparative study of Clerodendron inermes and Leucas cephalotes on Vishamajvara, Department of Dravyaguna, IPGT&RA, Jamnagar.
- Sudha Menon (2003): Clinical study of aetio-pathogenesis of AIDS and assessment of the efficacy of Indukanta Ghrita on its symptoms Jvara (pyrexia), Department of Roganidan & Vikriti Vigyan, IPGT&RA, Jamnagar.
- Rimpal Virsodiya (2006): Effect of Siddharthakadi Agada in the management of Malaria (Jvara), Department of Kayachikitsa, IPGT&RA, Jamnagar.
- Kapil Lathiya (2014): A study on Gomutrabhavita Pippali w.s.r to its antipyretic and analgesic activity, Department of Dravyaguna Vigyan, IPGT&RA, Jamnagar.
- Shweta R Vekariya (2015): Pharmacological evaluation of Mahanimba (Melia Azedarach Linn.) with special reference to analgesic and antipyrectic activities. Department of Dravyaguna Vigyan, IPGT&RA, Jamnagar.
Case reports and research updates
- In a study, 60 vishama jwara patients were selected. Out of which 24 patients were positive for malarial parasite test. The trial drug, Indrayavadi Vati was given in the dosage of 2-6gm for 7 days. After treatment, complete relief was observed in symptoms like headache, vomiting, nausea and rigors. Malarial parasite test was also negative after the treatment.[8]
- In another study on vishama jwara, 34 patients were treated with Leucas cephalotes (dronapushpi) in the dosage 3 -6 gm for 20 days. Total 76.47% of patients were completely cured.[9]
- Powder of Hymenodictyon excelsum (Bhramara Challika) was given to 25 patients of vishama jwara in a dosage of 2gm thrice a day for 5 – 15 days. This drug is found more effective in anyedyushka jwara than santata jwara.[10]
- Clerodendron inermes and Leucas cephalotes were given in dosage of 3gm for 10 days. Significant results were obtained on cardinal symptoms of jwara for both these drugs.[11]
- Total 23 patients with positive peripheral smear test for Plasmodium vivax were selected and treated with Siddharthakadi agada 3gm thrice a day for 1 week. Control group was treated with Chloroquine phosphate and Primaquine. Siddharthakadi agada has provided significant results in reducing the fever, rigor with chill, headache, bodyache, sweating, anorexia, weakness and cough. On comparison the patients treated with Siddharthakadi agada showed better results in controlling anorexia, headache and body ache. Peripheral smear test after seven days of treatment with agada was negative for all patients.[12]
- Powder of leaves and root of Melia Azedaracta Linn.(mahanimba) were administered to experimental models of induced pyrexia in albino rats. Root powder showed better antipyretic effect than leaf powder.[13]
Mechanism of action of antipyretic medicines
Inflammatory mediators released by peripheral mononuclear phagocytes and other immune cells induces fever. Fever inducing cytokines are transported from blood to brain. Prostaglandin E2 (PGE2) in the brain is believed to be the principle downstream mediator of fever. Inhibiting the production of PGE2 is a well known mechanism of antipyretics.[14]
Many drugs are reported to be having antipyretic action. A few of them are decoction and alcoholic extract of amlakyadigana (combination of Emblica officinalis Gaertn. (Amalaki), Terminalia chebulaRetz.(Haritaki), Piper longum L. (Pippali), and Plumbago zeylenica L. (Chitraka);[15] Aeginetia indica[16] , Grapevine leaf extract (Vitis vinifera)[17] , Cissampelos pareira Linn. , Cyclea peltata[18] and Guduchi ghrita.[14]
Controlled clinical trials of these medicines are required to establish their efficacy as treatment option to established anti pyretic drugs.
The treatment objective is not only to reduce body temperature, but also to maintain equilibrium of body components and preserve health.
Jwara in initial and acute stage with recent onset (less than seven days) is nava jwara. The dosha are afflicted with ama.
Synonyms: Taruna jwara, ama jwara, acute state
Clinical features
- Continuous features of jwara with or without rise in temperature and of acute onset
- Anorexia, indigestion, loss of appetite, excessive salivation, nausea, tastelessness in mouth, heaviness in stomach and in cardiac region; rigidity, numbness and heaviness of body.
- Constipation or passage of improperly formed stools, excessive urination.
- Presence of laziness and drowsiness without physical weakness.
- Absence of sweating [Cha.Sa.Chikitsa Sthana 3/133-136]
Management
Management principles
Therapeutic fasting after considering the strength of patient and severity of disease. This helps to promote digestion, transform ama(undigested toxins) and regain normal states of dosha[Cha.Sa.Chikitsa Sthana 3/140] Hot water, medicated gruels and herbs having bitter taste are prescribed to promote natural process of digestion and transformation of ama state [Cha.Sa.Chikitsa Sthana 3/142]
Medicinal preparations
Medicated water with six herbs (shadangapaniya):
Six herbs viz. Cyperus rotundus (musta), Fumaria parviflora (parpata), Chrysopogon zizanioides (ushira), Santalum album (chandana), Plectranthus vettiveroides (udichya) and Zingiber officinale (nagara) are boiled in water and then cooled. This water is prescribed for drinking. It helps to normalize body temperature and satisfy thirst. [Cha.Sa.Chikitsa Sthana 3/145]
Medicated gruels (yavagu):
Medicated gruels are prescribed after fasting. This dietary preparation is light to digest, promotes sweating, pacifies thirst and sustains vitality by providing nourishment. [Cha.Sa.Chikitsa Sthana 3/152] This can be continued for 6 days.
The medicated gruel is contraindicated in cases of excessive intake of alcohol, bleeding disorders especially through the upper orifices, in summer season and aggravation of pitta and kapha dosha.[Cha.Sa.Chikitsa Sthana 3/154] In such conditions, food including powdered roasted grains mixed with fruit juices, sugar or honey are prescribed for nourishment. [Cha.Sa.Chikitsa Sthana 3/155]
Panchakarma procedures
- Fomentation (swedana): Mild fomentation by using a thick blanket to cover body and induce sweating is advised. It removes obstruction in sweat pores, releases trapped body heat and promotes normal movement of dosha.
- Therapeutic emesis (vamana): It is indicated only in conditions of jwara with excessively aggravated kapha dosha. [Cha.Sa.Chikitsa Sthana 3/147]
Precautions in diet and lifestyle
In this stage, the patient shall avoid daytime sleep, head bath, external application of oils, sexual intercourse, direct exposure to wind, excessive physical activities, heavy to digest food, overuse of astringent and sweet taste, food items with hot potency and unctuous property, anger. [Cha.Sa.Chikitsa Sthana 3/138-39] [Cha.Sa.Chikitsa Sthana 3/195]
Jeerna jwara (Chronic stage)
Jwara lasting for more than seven days leading to a chronic disease is jeerna jwara. The acute stage is converted into chronic after therapeutic fasting is over and the dosha are not afflicted with ama state. [A.Hr.Nidana Sthana.2/56][4] Some opine a period of more than three weeks to term the condition as jeerna jwara [M.Ni.2/65][19]
Clinical feature
Presence of mild features of jwara with weak digestion.[M.Ni.2/65][19]
Pathogenesis
If the tolerance or immunity of body tissues (dhatu) is weak, the jwara affects them for a longer duration leading to chronic stage. [Cha.Sa.Chikitsa Sthana 3/291]
Management
Fasting is contraindicated in chronic stage. The weakened body tissues do not tolerate fasting. Therefore, nourishing and strength promoting diet is advised. [Cha.Sa.Chikitsa Sthana 3/292]
In chronic stage due to aggravation of vata and pitta dosha, internal administration of medicated ghee is recommended. [Cha.Sa.Chikitsa Sthana 3/164] The unctuous property and cold potency of medicated ghee pacifiers vata and pitta dosha. [Cha.Sa.Nidana Sthana 1/37]
Consumption of milk is also indicated in chronic stage. Choice of using it either hot or cold or processed with appropriate herbs depends on dominance of dosha in conditions. [Cha.Sa.Chikitsa Sthana 3/239]
Panchakarma procedures
Purification therapies are indicated in chronic stage, only if the patient does not respond to pacification therapies. [Cha.Sa. Chikitsa Sthana 3/168]
Therapeutic purgation (virechana): It is indicated only if the patient’s muscle mass, digestion and strength are not depleted. [Cha.Sa. Chikitsa Sthana 3/169]
Decoction enema (niruha basti): It is indicated in chronic debilitated conditions where therapeutic emesis (vamana) and purgation (virechana) are contraindicated. It promotes strength and power of digestion. [Cha.Sa.Chikitsa Sthana 3/170]
Unctuous enema (anuvasana basti): It is indicated in case of aggravation of vata dosha, depletion of kapha and pitta dosha. It is suitable for those having strong digestive power, but dry stools and difficulty in defecation. [Cha.Sa.Chikitsa Sthana 3/172-73]
Intranasal drug administration (nasya):It is indicated for patients having heaviness, headache and impaired sensoria. [Cha.Sa.Chikitsa Sthana 1/173-74]
Currently used herbal formulations:[20] Dashaashtanga churna, Samshamani Vati.
Currently used herbo-mineral formulations: Laghumalini vasant [R.T.S Kharaliya rasayana][21] Jeernajwarankusha rasa, Suvarnamalini vasanta [R.T.S Kharaliya rasayana][21], Arogyavardhini rasa [R.R.S Chapter 20][22].
Sannipata jwara (vitiation of all three dosha)
The condition of jwara in which all three dosha are vitiated simultaneously is known as “sannipata jwara”. [Cha.Sa.Nidana Sthana 1/29] The proportion of dosha involved in the pathogenesis may be different or equal based on exposure to causes.
General clinical features
Following are general clinical features observed in sannipataja jwara conditions:
Insomnia, giddiness, dyspnea, drowsiness, numbness, anorexia, thirst, fainting, rigidity, frequent sensation of burning and cold, cardiac pain, delayed response of transformation of dosha, insanity, blackish teeth, rough and blackish tongue; pain in joints, head and bones; crooked and dirty eyes; sticky eyelashes; tinnitus and pain in ears; delirium; inflammation of body channels; cooing sound; loss of consciousness; delayed elimination and depletion of sweat, urine and feces.[Su.Sa.Uttara Sthana.39/35-39][3]
Classification
The sannipataja jwara is presented in thirteen types of clinical presentations due to variable vitiated states of dosha. The clinical features are described as below:
| State of dosha | Clinical features* |
|---|---|
| Vata and pitta are codominant, while kapha is recessive | Giddiness, thirst, burning sensation, heaviness and excessive headache. |
| Vata and kapha are codominant, while pitta is recessive | Coldness, cough, anorexia, drowsiness, thirst, burning sensation and pain. |
| Pitta and kapha are codominant, while vata is recessive | Emesis, coldness, frequent burning sensation, thirst, unconsciousness and pain in the bones. |
| Vata predominant condition | Pain in the joints, bones and head; delirium, heaviness, giddiness, thirst and dryness of the throat as well as the mouth. |
| Pitta predominant condition | Blood in stool and urine, burning sensation, vomiting, disliking for doing any work, giddiness, drowsiness and cough. |
| Kapha predominant condition | Laziness, anorexia, nausea, burning sensation, vomiting, restlessness, giddiness, drowsiness and cough. |
| Kapha is excessively vitiated, pitta moderately vitiated and vata is less vitiated | Coryza, vomiting, laziness, drowsiness, anorexia and weak digestion. |
| Pitta is excessively vitiated, kapha moderately vitiated and vata is less vitiated | Yellowish discoloration of urine and eyes, burning sensation, thirst, giddiness and anorexia. |
| Vata is excessively vitiated, kapha moderately vitiated and pitta is less vitiated | Headache, trembling, breathlessness, delirium, vomiting and anorexia. |
| Kapha is excessively vitiated, vata moderately vitiated and pitta is less vitiated | Coldness, heaviness, drowsiness, delirium and excessive pain in bones as well as head. |
| Vata is excessively vitiated, pitta moderately vitiated and kapha is less vitiated | Dyspnea, cough, coryza, dryness of the mouth and excessive pain in the flanks. |
| Pitta is excessively vitiated, vata moderately vitiated and kapha is less vitiated | Diarrhea, weak digestion, thirst, burning sensation, anorexia and giddiness. |
| All the three doshas vitiated to equal extent | Patient has feeling of burning sensation sometimes and sometimes feeling of cold; Pain in the bones, joints and head; Eyes are with excessive lacrimation, dull, reddish with eyeballs protruded out; Ringing sound and pain in the ears; Pricking pain in throat like thorn of grain; Drowsiness, delusion, delirium, cough, breathlessness, anorexia and giddiness; Burning sensation of tongue, and turns rough to touch; Excessive fatigue; Spitting of blood and bile mixed with phlegm (sputum); Swaying movements of head, thirst, sleeplessness and pain in the cardiac region; Sweat, urine and stool reduced in amount with delayed evacuation; Body is not excessively emaciated (due to accumulated dosha); Makes cooing sound constantly; Urticaria and bluish-black or reddish circular patches appear on the skin; Patient speaks less or unable to speak; Inflammation of passages; Heaviness in the abdomen; The dosha return to its ama free state or normal state after a very long time. |
- [Cha.Sa.Chikitsa Sthana 3/91-109]
Abhinyasa/hataujasa jwara
The specific condition of sannipata jwara in which ojas is affected is known as hatojasa jwara or abhinyasa jwara. It is presented with following clinical features:
Moderate rise in body temperature, lowered state of consciousness, illusion, feeble voice, rough tongue, sore throat, absence of sweating, constipation, watering of eyes, cardiac pain, aversion to food, loss of luster and the person lies down panting, delirium and other complications. [Su.Sa.Uttara Sthana.39/39-40][3]
This condition is difficult to cure.
| Cardinal feature | Type of sannipatajwara |
|---|---|
| Excessive sleep | Abinyasa |
| Weakness or wasting | Hataujasa |
| Immovable limbs | Sanyaasa |
- [Su.Sa.Uttara Tantra 39/42][3]
Prognosis
Sannipata jwara is incurable or difficult to cure if functions of dosha are obstructed, digestive capacity is very poor, and the condition is severe with presence of all clinical features.[A.Hr.Nidana Sthana.2/34][4]
Sannipata jwara associated with development of swelling at the parotid site (root of ear) is incurable. [Cha.Sa.Chikitsa Sthana 3/287]
Principles of management
The sannipata jwara is managed with following principles:
- Improve the state of depleted dosha (by use of property, action, or substances similar to that dosha)
- Decrease the state of aggravated dosha (either by pacification or by purification treatments)
- Target the sites of kapha dosha primarily [Cha.Sa.Chikitsa Sthana 3/286-87]
Vishama jwara
The condition of jwara in which intermittent or irregular clinical features are observed with episodes is known as ‘vishama jwara’. The fundamental cause lies in the episodic or opportunistic aggravation of dosha involved in the pathogenesis.
Causes and pathogenesis
If the initial stage of jwara is not treated well, and aggravated dosha are not evacuated properly, then the dosha reside in dormant state in the body channels. Whenever the person is exposed to etiological factors and/or to exogenous causes, the same opportunistic dosha are aggravated to cause vishama jwara. [Cha. Sa. Chikitsa Sthana 3/292] The episodes of vishama jwara are precipitated during favorable conditions of the dosha to exhibit its signs and symptoms. When the precipitating factors are absent, dosha lose their strength, and again attain dormant state at their respective site.[Cha.Sa.Chikitsa Sthana 3/70]
The episodic clinical presentation is due to the other variable factors like time, body constitution, digestive capacity etc.[Su.Sa.Uttara Sthana.39/124][3]
This is similar to a seed germinates in fertile soil only at a time when it gets proper nourishment, in proper season. Similarly, the dormant dosha cause disease only when they get favorable vitiating factors and strength of opposing factors (host defense) is depleted. [ Cha.Sa.Chikitsa Sthana 3/68-69]
General clinical features
Irregular onset, irregular symptoms and irregular time of appearance may stay for longer duration in vishama jwara. [A.Hr.Nidana Sthana 2/69][4]
| Type of vishama jwara | Site | Tissue (dhatu) involved | Pattern of clinical presentation |
|---|---|---|---|
| Santata | - | Rasa dhatu (nutritive fluid), Rakta dhatu (blood) | Continuously present for 7, 10 or 12 days |
| Satata | Stomach | Rakta dhatu (blood) *, Rasa dhatu (nutritive fluid)# | Twice in 24 hours |
| Anyedyushka | Chest | Meda dhatu (adipose tissue) *, Mamsa dhatu (muscle tissue) # | Once in 24 hours |
| Tritiyaka | Throat | Asthi dhatu (bone tissue)*, Meda dhatu (adipose tissue) # | Every third day (gap of one day) |
| Chaturtaka | Head | Majja dhatu (bone marrow)*, Asthi dhatu (bone tissue) # | Every fourth day (gap of two days) |
| Chaturtakaviparyaya | - | Asthi dhatu and Majja dhatu (bone & bone marrow) * | Continuous for two days (gap of one day)$ |
*[Cha.Sa.Chikitsa Sthana.3/61-62, 73], #[Su.Sa.Uttara Sthana 39/83-88], $[M.Ni.2/39][19]
Dosha specific presentations
Tritiyakajwara (every third day)
It affects different body parts depending on dosha specific aggravation as below:
- When kapha and pitta dosha are aggravated, it afflicts the sacral region (trika).
- When the vata and kapha dosha are aggravated, the upper back (prishtha) is affected.
- The head region is affected in the case of aggravation of vata and pitta dosha. [Cha.Sa.Chikitsa Sthana 3/71]
Chaturthakajwara (every fourth day)
If kapha dosha is affected, then the calf region is affected initially. In case of vata dominancy, head region is affected. [Cha.Sa.Chikitsa Sthana 3/72]
Viparyaya vishamajwara
If vitiated dosha is situated in two or more than two sites of kapha dosha, it leads to viparyaya vishamajwara. [Su.Sa.Uttara Sthana.39/55][3]
If dosha is present in chest and stomach, it causes continuous jwara, which remits once in forenoon.
Dosha present in throat, chest and stomach cause jwara, which remits on third day. Dosha in head, throat, chest and stomach, produces jwara, which remits on fourth day.
Vatabalasaka jwara
It is characterized by continuous mild jwara, dryness, edema and rigidity in body.[M.Ni.2/40][19] If vata and kapha are present in the skin, it causes rigor in the beginning and when they subside, pitta causes burning sensation and vice versa. [Su.Sa.Uttara Sthana.39/59][3]
Pralepaka jwara
The person experiences mild jwara associated with heaviness and heat all over body. [M.Ni.2/41][19] It is caused by aggravated kapha and pitta.
Prognosis
Santata jwara is extremely difficult to treat. [Cha.Sa.Chikitsa Sthana 3/55]
Management
The management depends on dominance of dosha in the conditions.
If vata is predominant in tritiyaka and chaturtakajwara, it is managed by the administration of ghee, medicated unctuous and non-unctuous enema. The diet and drinks administered should be hot in potency and unctuous.
If pitta dosha is predominant, therapeutic purgation (virechana) is advised. Medicated ghee and milk can be given. The diet should be cold in character and bitter in taste.
Kapha predominant vishama jwara is managed through therapeutic emesis (vamana). Fasting, administration of hot decoction and digestive medicines are done. Diet and drinks should not be unctuous in nature. [Cha.Sa.Chikitsa Sthana.3/293-96]
Commonly used herbs:
Phyllanthus emblica (amalaki), Terminalia bellirica (bibhitaki), Terminalia chebula (haritaki), Picrorhiza kurroa (katukarohini), Trichosanthes cucumerina (patola), Swertia chirayata (kiratatikta), Holarrhena pubescens (vatsaka).
Medicated ghee: Shatpala grita [A.Hr Chikitsa Sthana 5/22-23][4], Kalyanaka grita [A.Hr Uttara Tantra 6/26-31][4], Tiktaka grita [A.Hr Chikitsa Sthana 19/2-6][4]
Panchakarma procedures:
- Fumigation with medicines like Aparajitadhuma [A.Hr.Chikitsa Sthana.1/164][4]
- Therapeutic emesis with ghee in maximum dose. [A.Hr. Chikitsa Sthana 1/159][4]
- If jwara is not responding by the above said procedures, venesection (raktamokshana)is indicated. [A.Hr.Chikitsa Sthana.1/166][4]
Specific formulations for five types:
The five types of vishama jwara are managed by five decoctions made from drugs described below:
- In santatajwara, Kalingaka, patola leaves and katukarohini
- In satatajwara, Patola, sariva, musta, patha and katukarohini
- In anyedyushkajwara, Nimba, patola, triphala, mrudvika, musta and vatsaka
- In tritiyaka jwara, Kiratatikta, amrita, chandana, vishvabheshaja
- In chaturthaka jwara, Guduchi, amalaka and musta. [ Cha.Sa. Chikitsa Sthana 200-203]
| Type | Medicine |
|---|---|
| Santata | Lakshminarayana rasa [R.T.S Kharaliya rasayana][21], Laxmivilasa rasa [B.R 5/1223-35][6], Guduchyadi kwatha [B.R 5/156][6], Drakshadi churnam |
| Satata/ Anyedyushka/ Tritiyaka/ Chaturthaka | Mallasinduramisranam [R.T.S Kupipakwa prakarana][21], Gandhaka druti[22], Tiktaka kwatha |
- [Chikitsapradeepa][23]
Rasayana therapy:
Vardhamanapippali rasayana [Cha.Sa.Chikitsa Sthana 1/3/36] to prevent recurrence is advised.
Jwara affecting body tissues (dhatugata jwara)
When jwara affects body tissues, it produces tissue specific clinical features. These conditions of lodging pathogenic factors of jwara at different tissues (dhatu) are termed as ‘dhatugata jwara’. This suggests progressive stages of disease affecting deeper tissues.[Cha.Sa.Chikitsa Sthana 3/75-82] [Su.Sa.Uttara Sthana.39/83-88][3]
Jwara affecting nutrient fluids (rasa dhatu)
Clinical features
Heaviness, miserable feeling, anxiety, exhaustion, vomiting, anorexia, increase in external temperature, body ache and yawning
Treatment of choice
Therapeutic emesis (vamana) and fasting (langhana)[Cha.Sa.Chikitsa Sthana.3/315-17]
Drug of choice: Piper longum (pippali) [20]
Jwara affecting Blood (rakta dhatu)
Clinical features
Increase in body temperature, eruptions, thirst, frequent hemoptysis, burning sensation, discoloration, giddiness, intoxication and incoherent speech
Treatment of choice
External application of medicaments like pouring decoctions and anointing medicines over body [Cha.Sa.Chikitsa Sthana 3/315-17]
Drug of choice: Hemidesmus indicus (sariva) [20]
Jwara affecting Muscle tissue (mamsa dhatu)
Clinical features
Internal feeling of burning, thirst, unconsciousness, weakness, diarrhea, bad body odor and abnormal muscle movements like throwing away limbs
Treatment of choice
Therapeutic purgation (virechana) and fasting [Cha.Sa.Chikitsa Sthana 3/315-17]
Drug of choice: Tinospora cordifolia (guduchi) [20]
Jwara affecting Adipose tissue (meda dhatu)
Clinical features
Excessive sweating, thirst, incoherent speech, frequent vomiting, inability to tolerate own body odor, fatigue and anorexia
Treatment of choice
Therapeutic purgation (virechana) and fasting [Cha.Sa.Chikitsa Sthana 3/315-17]
Drug of choice: Azadirachta indica (nimba) [20]
Jwara affecting Bone tissue (asthi dhatu)
Clinical features
Diarrhea, emesis, pain in the bones, cooing sound (kujana), convulsive movements of the body and limbs, dyspnea
Treatment of choice
Decoction enema and untuous enema [Cha.Sa.Chikitsa Sthana 3/315-17]
Drug of choice: Triphala (Terminalia chebula, Treminalia bellirica and Phyllanthus emblica) [20]
Jwara affecting Bone marrow (majja dhatu)
Clinical features
Hiccup, severe dyspnea, cough, feeling of entering into darkness frequently, cutting pain in the vital organs (marma), feeling of cold externally and internal burning sensation
Treatment of choice
Decoction enema and untuous enema [Cha.Sa.Chikitsa Sthana 3/315-17]
Drug of choice: Iron (lauha) [20]
Jwara affecting Reproductive fluid/semen (shukra)
Clinical features
Rigidity of penis, ejaculation and destruction of semen resulting in the extinction of life
Treatment of choice
Incurable [Cha.Sa.Chikitsa Sthana 3/315-17]
Prognosis
Jwara at the site of nutrient fluid (rasa), blood (rakta), muscle (mamsa) and adipose tissue (meda dhatu) are curable. Jwara affecting bones (asthi dhatu) and marrow (majja dhatu) are difficult to cure. Jwara affecting semen/reproductive fluid (shukra dhatu) is incurable. [Cha.Sa.Chikitsa Sthana.3/83]
Abbreviations
Cha. = Charak, Su. = Sushruta, A. = Ashtanga, S. = Sangraha, Hr. = Hridayam, Sa. = Samhita, M.Ni = Madava Nidana, R.T.S = Rasatantrasara and Siddhaprayoga sangraha, R.R.S = Rasaratnasamucchaya, B.R = Bhaishajya ratnavali
Related chapters
Send us your suggestions and feedback on this page.
References
- ↑ http://namstp.ayush.gov.in/#/sat
- ↑ Walter EJ, Hanna-Jumma S, Carraretto M, Forni L. The pathophysiological basis and consequences of fever. Crit Care. 2016;20(1):200. Published 2016 Jul 14. doi:10.1186/s13054-016-1375-5
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 3.13 3.14 3.15 3.16 3.17 3.18 3.19 3.20 3.21 3.22 3.23 3.24 3.25 Sushruta. Sushruta Samhita. Edited by Jadavaji Trikamji Aacharya. 8th ed. Varanasi: Chaukhambha Orientalia;2005.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 Vagbhata. Ashtanga Hridayam. Edited by Harishastri Paradkar Vaidya. 1st ed. Varanasi: Krishnadas Academy;2000.
- ↑ Nishteswar K, Vidyanath R, Sahasrayogam, Kashaya kalpana, In:Nishteswar K , Vidyanath R, Editor. Sahasrayoga. Varanasi: Chowkhamba Sanskrit Series Office; 2014.p.4
- ↑ Madavji Trivikramji Acharya. Rasamrutam. Chapter 9 Rasayogavignaniya adhyaya, Verse 80-81
- ↑ Dal D K: Vishamajvara (malaria) chikitsatmakaadhyayana, Department of Kayachikitsa and Panchakarma, IPGT&RA, Jamnagar. MD Thesis, 1981
- ↑ Kashaih M (1983): A study on effect of certain indigenous drug in Vishamajvara, Department of Kaumarabhritya, IPGT&RA, Jamnagar
- ↑ Sarvaiya D B (1987): Dravyavigyana of Bhramara-Challika and its therapeutic effect on Vishamajvara,Department of Dravyaguna, IPGT&RA, Jamnagar
- ↑ Varsha Solanki (1998): A comparative study of Clerodendron inermes and Leucas cephalotes on Vishamajvara, Department of Dravyaguna, IPGT&RA, Jamnagar
- ↑ Rimpal Virsodiya (2006): Effect of Siddharthakadi Agada in the management of Malaria (Jvara), Department of Kayachikitsa, IPGT&RA, Jamnagar.
- ↑ Shweta R Vekariya (2015): Pharmacological evaluation of Mahanimba (Melia Azedarach Linn.) with special reference to analgesic and antipyrectic activities. Department of Dravyaguna Vigyan, IPGT&RA, Jamnagar.
- ↑ 14.0 14.1 Ashok BK, Ravishankar B, Prajapati PK, Bhat SD. Antipyretic activity of GuduchiGhrita formulations in albino rats. Ayu. 2010 Jul;31(3):367-70. doi: 10.4103/0974-8520.77162. PMID: 22131741; PMCID: PMC3221073
- ↑ Timbadiya MJ, Nishteswar K, Acharya R, Nariya MB. Experimental evaluation of antipyretic and analgesic activities of AmalakyadiGana: An Ayurvedic formulation. Ayu. 2015 Apr-Jun;36(2):220-4. doi: 10.4103/0974-8520.175554. PMID: 27011727; PMCID: PMC4784136
- ↑ Reza MS, Jashimuddin M, Ahmed J, Abeer M, Naznin NE, Jafrin S, Haque ME, Barek MA, UdDaula AFMS. Pharmacological investigation of analgesic and antipyretic activities of methanol extract of the whole part of Aeginetia indica. J Ethnopharmacol. 2021 Feb 7;271:113915. doi: 10.1016/j.jep.2021.113915. Epub ahead of print. PMID: 33567308
- ↑ Aouey B, Samet AM, Fetoui H, Simmonds MSJ, Bouaziz M. Anti-oxidant, anti-inflammatory, analgesic and antipyretic activities of grapevine leaf extract (Vitis vinifera) in mice and identification of its active constituents by LC-MS/MS analyses. Biomed Pharmacother. 2016 Dec;84:1088-1098. doi: 10.1016/j.biopha.2016.10.033. Epub 2016 Oct 22. PMID: 27780137.
- ↑ Singh SG, Nishteswar K, Patel BR, Nariya M. Comparative antipyretic and analgesic activities of Cissampelos pareira Linn. and Cycleapeltata (Lam.) Hook. F. & Thomas. Ayu. 2016 Jan-Mar;37(1):62-66. doi: 10.4103/ayu.AYU_208_14. PMID: 28827957; PMCID: PMC5541469
- ↑ 19.0 19.1 19.2 19.3 19.4 Madhavakara. Madhava Nidanam (Roga vinischaya). Translated from Sanskrit by K. R. Srikantha Murthy. 8th ed. Varanasi: Chaukhambha orientalia;2007
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 Jwara. In: Ranade S,ed.1 Kayachikitsa.Delhi: Chaukhamba Sanskrit pratishthan; 2005
- ↑ 21.0 21.1 21.2 21.3 Krishnanand Maharaj. Rasatantrasara and Siddhaprayoga sangraha. 15th ed. Kalera-Krishna Gopal: Krishnagopal Ayurved Bhavan:2001
- ↑ 22.0 22.1 Vagbhata, Rasa ratna samucchaya. Edited by Ambikadatta Sastri. 9th ed. Varanasi: Chaukhambha Amarabharati Prakashan; 1995
- ↑ Gokhale B.V. Jwararoga.In: Chikitsapradeep.Pune:Dhanwantary Pratishthan;1989:1-3.