Difference between revisions of "Vaitarana Basti"
| Line 299: | Line 299: | ||
[[File:Nervous systems.jpg|center]] | [[File:Nervous systems.jpg|center]] | ||
There may be possible correlation - | There may be possible correlation - | ||
| − | * It modulates endocrine functions ( | + | * It modulates endocrine functions (myoenteric plexus—ANS—Brain—Pituitary—Adrenal ovarian/testicular axis). |
| − | * It | + | * It may cause pressure variation of intestinal mucosa, which may induce difference in intestinal intra- cellular and extra -cellular fluid. |
* It acts by a curious bio feedback mechanism yet to be identified. | * It acts by a curious bio feedback mechanism yet to be identified. | ||
Basti dravya reaches up to micro & macro levels due to its virya(potency). It helps first to disrupt the pathogenic process & carries the morbid matter towards the colon (pakwashaya) for elimination. Thus, it acts as a curative as well as purification measure. | Basti dravya reaches up to micro & macro levels due to its virya(potency). It helps first to disrupt the pathogenic process & carries the morbid matter towards the colon (pakwashaya) for elimination. Thus, it acts as a curative as well as purification measure. | ||
Revision as of 05:16, 22 November 2022
Vaitarana basti is a therapeutic enema. It is effective in diseases like amavata, katishoola (lumbago), gridhasi (sciatica), klaibya (sexual dysfunction), vishama jwara(fever) etc. The description is available in ayurveda texts like Chakradutta, Vranda madhava, Vangasena samhita. In current scenario, it is used in amavata patients as a safe, innocuous & custodian therapy for the patient. It is also useful in ama dosha predominant conditions like anaha (abdominal distension), shotha (swelling), shula (pain). It has vata-kapha pacifying properties and helps in removing avarana of vata by kapha. The present chapter describes advantages and practical aspects of vaitarana basti.
| Section/Chapter/topic | Concepts & Practices/Basti/Vaitarana Basti |
|---|---|
| Authors | Patil Rajkala P.1, Gupta Rishanki2 |
| Reviewer | Basisht G.3, |
| Editor | Deole Y.S.4 |
| Affiliations |
1Department of Panchakarma, Faculty of Ayurveda, I.M.S., B.H.U., Varanasi, India 2Department of Rog Nidana, Faculty of Ayurveda, I.M.S., B.H.U., Varanasi, India 3Rheumatologist, Orlando, Florida, U.S.A. 4Department of Kayachikitsa, G.J.Patel Institute of Ayurvedic Studies and Research, New Vallabh Vidyanagar, Gujarat, India |
| Correspondence emails |
rajkalapatil@bhu.ac.in, carakasamhita@gmail.com |
| Publisher | Charak Samhita Research, Training and Development Centre, I.T.R.A., Jamnagar, India |
| Date of publication: | November 18, 2022 |
| DOI | In process |
Etymology and derivation
According to Padma Purana, Vaitarana means ‘Vai’ (meaning truly) to ‘tarana’ (means saving). Vaitarana is the enema which saves life by preventing many diseases. It means to donate, go across, to leave which helps to expel the dosha. Vaitarana is the name of river, which can bring back the dead to live. It is meant to cross a river, transporting (a departed spirit) over the river that flows between earth and the lower regions [Monnier-Williams Sanskrit-English Dictionary, 1899]. Hence, this basti is so powerful that it can bring back life of a person, who is about to die. The first reference regarding vaitarana basti is probably found in the Siddhayoga or Vrindamadhava ; narrated as separate section as this formulation does not satisfy inclusion in description of niruhabasti. The critical edition of Vrindha Madhava by Dr.Premavati Tiwari and Dr. Asha Kumari reports a variant reading where guda (jaggery) is replaced by hingu (Ferula asafoetida).[1]
The basic difference in niruha and vaitarana basti as follow-
| Niruha Basti (purification enema) | Vaitarana Basti (Vaitarana enema) |
|---|---|
| Contents- Makshika (honey), Lavana (salt), Sneha (oil), Kalka(paste), &Kwatha(decoction)[2]. | Contents- Saindhava (rock salt), Guda (jaggery), Chincha (tamarind), Taila (oil), & drava dravya (liquids). |
| Makshika(honey) | Instead of Makshika(honey) ;Guda(jaggery) is there. |
| Here kalka(paste) mainly of shatapushpa (dill seed) or madanaphala (emetic nut). | chincha(tamarind) act as kalka (paste). |
| sneha(oil) | here rukshna sneha(oil processed with herbs of hot potency and dry property that will not increase kapha) used like brihat saindhavadi taila (special medicated oil). |
| Generally used kwatha (decoction) like dashmoola (group of ten herbs). | Here gomutra(cow urine) used instead of any kwatha (decoction). |
| Contents | Chakradutta | Vrindhamadhava | Vangasena | Weight in grams/ml |
|---|---|---|---|---|
| Saindhava (rock salt) | 1 karsha | 1 karsha | 1 karsha | 10 gms |
| Guda (jaggery) | 1 shukti(1/2 pala) | 1 shukti(1/2 pala) | 1/2 pala | 25 gms |
| Amlika (tamrind) | 1 pala | 1 pala | 1 pala | 50 gms |
| Gomutra (cow urine) | 1 kudava(4 pala) | 1 kudava(4 pala) | Ishattaila | 200 ml |
| Godugdha (cow milk) | Not mentioned | Not mentioned | 1 kudava | - |
| Taila(–ilataila- sesame oil) | Quantity not mentioned | Oil insmall quantity | Oil in small quantity | 10-25 ml |
| Sr.No | Contents | Botanical /English name | Rasa (Taste) | Virya (Potency) | Vipaka (metabolic properties- after digestion) | Guna | Properties | Chemical constituent |
|---|---|---|---|---|---|---|---|---|
| 1. | Amlika | Tamarindus indica (fam. Fabaceae)/ Tamarind | Amla | Ushna | Amla | Guru, Ruksha, Sara. | Kaphavatanut, Dipana, Bastisuddhikara, | Tamarindica, saponin, sugar, inorganic acid. |
| 2. | ErandTaila | Ricinus Communis/ Castor Oil | Madhura,Katu, Kashaya (Sweet, pungent, Astringent) | Ushna (Hot) | Madhura (Sweet) | Snigdha, Guru, Sukshma, Vyavayi, Vishada,Sara,Vikasi. | Shool, Shothain kati, Vrsya, Amavatahara, VataKaphahara and Adhobhagadoshahara (disorders of lower parts of the body) | - |
| 3. | Saindhava | Rock salt | Madhura | Shita | - | Laghu | Srotosodhaka | NACL |
| 4. | Gomutra | Cow’s urine | Katu | Ushna | - | Laghu, Tikshna | Vatanulomana, Srotosodhak | Urea,Uric acid |
| 5. | Guda | Saccharin offcinarum (fam.poaceae)/ Jaggery | Madhura | Ushna, Natishita | Madhura | Snigdha, Ishatksariya. | Vata-Pitta Nashaka. Saktasochana, Vrsya, Vataghna-Natipittajit- -Kaphavrddhikara, Krmivrddhikara, Balya, Medovrddhikara |
sugar |
Indications
- Shoola (pain),
- Anaha (gaseous distention),
- Amavata (diseases due to Ama and Vata)
- Shopha of kati, uru, prushta(inflammation of upper or lower back)
- Urusthambha (specific diseaseof lower limb)
- Gridhrasi (sciatica)
- Janu samkocham (stiffness in Knee)
- Vishama jwara(fever)
- Klaibya (impotency)
Method of preparation
A) Materials Required to Formulate Basti.
- Basti putak (enema bag)
- Basti netra (nozzle)
- Gloves
- Cotton cloth
- Mortal & pastel
B)Ingredients of basti
- Guda (jaggery)
- Saindhava lavana(rock Salt)
- Gomutra (cow urine) ( or arka fresh urine is not available)
- Chincha (tamarind)
- Erand taila (castor oil)
C)Procedure to formulate & administration of basti
Pre-procedure:
a) Preparation of patient
b) Preparation of basti.
a) Preparation of patient: After the evacuation of bladder and bowels, local massage and fomentation on pelvic region shall be done.
b) Preparation of basti: Vaitarana basti is prepared as per the classical method used for the preparation of niruha basti. Jaggery (guda) is mixed uniformly with a small amount of lukewarm water. Saindhava is added to the above. Tila taila is added till the mixture become homogenous. Chincha kalka is prepared with warm water and added to the above mixture carefully. Gomutra is added slowly and mixing is continued so as to have uniform basti dravya. Finally, after filtering, basti dravya is made lukewarm by keeping it into hot water bath.
Main procedure (pradhana karma):
Patient is advised to lie down in the left lateral position on the basti table with straight body and left hand kept below head. His right leg is folded at knee joint and made to rest flat over the straight left leg. Then lukewarm (sukhoshna) unctuous material (sneha) is applied to the anal region and on the basti instrument (Netra). It is inserted slowly up to 1/4 part of the bastinetra. Lukewarm basti should be administered slowly.Post procedure (pashchat karma):
The basti instrument is removed from anus. Then gentle tapping on thigh & buttocks is done. Then the patient is asked to change posture to left lateral. If patient gets natural urge within 10 to 30 minutes, he will be advised to evacuate bowels.Clinical features of proper basti karma are observed.Basti retention time (pratyagamana):One muhurta (48 minutes).
Clinical features after administration:
Proper dose
- Prashasta vidamutra (proper amount of defecation, urination & evacuation of flatus)
- Agni vriddhi (improves digestion)
- Ruchi (increased desire to take food)
- Ashaya laghvani (lightness in body)
- Roga upshanti (resolution of disease state)
- Bala vriddhi(increased physical strength).
Less dose
- Shiro hridaya, guda basti, medhra vedana(pain in head, heart, anal region, urinary bladder, penis)
- Shopha (swelling)
- Pratishyaya(rhinitis)
- Parikartika(fissure)
- Hrillasa (nausea)
- Maruta mutra sanga(retention of flatus & urine)
- Shwasa (dyspnea).
Excess dose
- Kapha pitta kshaya (reduction of kapha & pitta)
- Anil prakopa (increment of vata)
- Angamarda (body pain)
- Klama (fatigue)
- Vepana (trembling)
- Nidra-balaabhava(absence of sleep & strength)
- Tamapravesha(blackouts)
- Hikka(hiccup)
- Unmada (insanity)
- Adhmana(bloating)
- Parikartika(fissure)
- Stambha(stiffness)
- Kamala(jaundice)
D) Time of administration
Vaitarana basti can be given after meal also.
Mode of action of basti
Basti introduced into the rectum (pakwashaya) acts upon the whole body and on every system of the body. It draws out impurities from head to toe by its potency just as the sun evaporates water from the earth by its heat. [Cha.Sa. Siddhi Sthana 7/64] As the cloth absorbs the dye from water mixed with kusumba(safflower) plant, in the same way Basti eliminates the mala from the body which have undergone liquefaction due to snehana and swedana. [A. Hru. Sutra Sthana 19]
The basti dravya churns and collects the accumulated dosha and stool (shakrut) from umbilical, hypogastric and pelvic region (nabhi, kati, parshwa and kukshi pradesha), causes oleation (snehana) to the body and expels out the dosha. [Cha. Sa. Siddhi Sthana 1/40]
Mode of action ofvaitaranabasti:
Note: The pharmacological properties of ingredients after their rectal administration are not yet studied. The properties of ingredients after oral administration are studied and presented here for reference.
Saindhava lavana (rock salt): Saindhava lavana is the purest form of rock salt, considered the best among all varieties of salt and advisable for daily consumption. It possesses 85% NaCl and 15% trace materials, whereas another salt contains 97% NaCl. It is salty and slightly sweet in taste; madhura vipaka (sweet post digestive effect), sheeta veerya (cold potency), light to digest and unctuous in nature. In basti therapy, rock salt is added to prepare an emulsion. It helps to dissolve and expel dosha from the intestines.[4]
The role of subtle (sukshma), unctuous (snigdha) and sharp (tikshna) properties are as below:
- - By virtue of subtle (suskhma guna), basti dravya reaches up to the molecular level. It helps to pass the drug molecule in systemic circulation through the mucosa.
- - Sharp (tikshnaguna) breaks down the morbid mala & dosha bondings (sanghata), hence helpful for the elimination of waste due to its irritant property.
- - Unctuous (snigdhaguna) is capable of liquefying the dosha and breaking it into minute particles.
Chincha / Tamarind (Tamarindus indica L.) :
Oral administration of chincha has vata-kapha pacifying, dry (ruksha) and hot (ushna) properties. These are useful in management of amavata. Tamarind is rich in tartaric acid which is a potent antioxidant and is a good source of iron and thiamine. The ripe fruit of tamarind is madhura-amla (sweet-sour) in taste. It is heavy to digest (guru),dry (ruksha),and hot in potency (ushna veerya) with sour (amla) post digestive effect (vipaka).
Ripe fruit pacifies vata and pitta. It has appetizing, digestive, thirst suppressing liver stimulant, anti-inflammatory, diuretic, anti-toxic, bladder purifying, anti-fatigue actions. It is useful for fever, constipation, loss of appetite, wound, sunstroke, rheumatism, inflammation, and diabetes. Its fruit is laxative. Leaves are useful to destroy parasitic intestinal worms. It is used as a food and has culinary uses. It is made into a refreshing and cooling beverage particularly used in fever. It possesses antioxidant, anti-inflammatory, anti-microbial, anti-fungal, anti-viral, hepato-protective, anti-nematidal, molluscicidal, antidiabetic, anti-cytotoxic activities.[5][6]
Tamarind fruit has anti spasmolytic activity by blocking calcium channel has a laxative effect due to the presence of malic acid, tartaric acid and potassium and it prevents cardiovascular diseases and obesity due to the content of polyphenol and flavonoids in it.[7]
Jaggery: In vaitarana basti, jaggary is used instead of honey (madhu). Saindhava along with jaggary makes a homogenous mixture, to form a solution having properties to permeable the water easily. The retention of the irritative substances may be favored by making its solution as nearly isotonic as possible by using colloidal fluids as a combination of this basti dravya, it also helps in carrying the drug into the micro-cellular level. It also contains polyphenols, a phenolic compound with antioxidant and cytoprotective activities. Jaggery is a very useful substance for oedema patient, when it is consumed along with ardraka, abhaya, sunthi, or pippali. It is also good for the patients with dysuria, constipation, cardiac problems, asthma, allergies, chronic fever, piles, throat and lung infections, malabsorption syndrome (grahani) and kapha vataja roga. [8][9]
Gomutra (cow urine): In vaitarana basti, cow urine is main ingredient. Its pungent taste (katu rasa), pungent post digestive effect (katu vipaka), hot potency (ushna veerya), light to digest (laghu), dry (ruksha) and sharp (tikshna) properties pacify kapha and vata. It stimulates agni (agnideepana-pachana), purifies body channels (srotovishodhana),pacifies vata (vatanulomana) and relieves ama. It is the best and useful among all urines (mutra).[10] It is useful in obesity, certain cardiac and renal diseases,indigestion, stomachache, diarrhea, oedema, jaundice,anemia, hemorrhoids and skin diseases including vitiligo. It acts as bio-enhancer and has antifungal, antimicrobial, germicidal, bactericidal, anthelmintic, antioxidant and antineoplastic action. It is useful in hypersensitivity reactions and in numerous other diseases including increasing the life span of a person. It has immune enhancer properties. It augments B and Tblastogenesis and IgA, IgG, and IgM titer in experimental animals. It exhibits antimicrobial and germicidal activity due to the presence of urea, creatinine, and Arum hydroxide (wwarnakshara) in it.Its anti-cancerous activity is due to the presence of uric acid and Allantoin in it. It shows wound healing activity due to the presence of allantoin, immunomodulation due to presence of Arum hydroxide. It prevents cardiovascular diseases due to the presence of kallikrein, urokinase, hippuric acid and ammonia in it. It attributes anti-obesity properties due to the content of copper. It exhibits anti-toxic activity by virtue of Arum hydroxide present in it.[11]
Tilataila(Sesame oil): In vaitaranbasti, sesame oil is mixed with the solution of jaggary and saindhavato form uniform mixture.
Probable mode of action
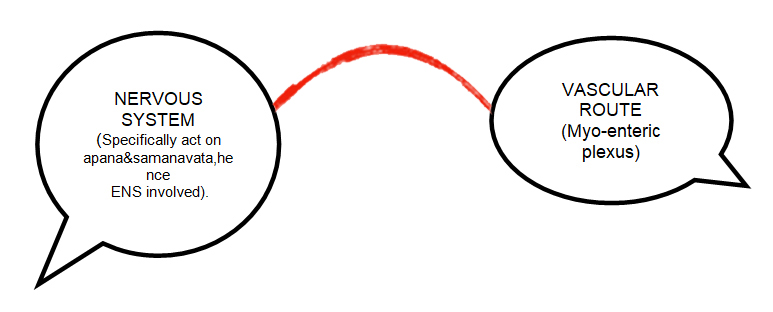
It may act through vascular route(myo-enteric venous plexus),nervous route(specifically act on apana&samanavata,hence ENS involved).
There may be possible correlation -
- It modulates endocrine functions (myoenteric plexus—ANS—Brain—Pituitary—Adrenal ovarian/testicular axis).
- It may cause pressure variation of intestinal mucosa, which may induce difference in intestinal intra- cellular and extra -cellular fluid.
- It acts by a curious bio feedback mechanism yet to be identified.
Basti dravya reaches up to micro & macro levels due to its virya(potency). It helps first to disrupt the pathogenic process & carries the morbid matter towards the colon (pakwashaya) for elimination. Thus, it acts as a curative as well as purification measure.
practical application
The practical applied aspect of vaitaranibastiis described as follows:
A) Pre-requisites for formulation of basti: The following points should be in consideration to have good results;
- - Tamarind paste (Chincha kalka):The tamarind paste is prepared after removing fiber and seeds from it. Actual weight of this paste is measured. Tamarind (chicha) should be soaked in water(room temperature) overnight, then fibrous & seed part extracted & remaining portion should be filtered with the help of fine cotton cloth. In case of instant preparation, the tamarind can be used after soaking it in hot water for fifteen minutes. Tamarind (chincha) should be old (purana), blackish in texture; should not having whitish coated texture.
- - Jaggery: It should be use in melted form(semiliquid preparation). Jaggery should be added with 3-4ml hot water, mixed gently & then should be filtered out.It should not be grinned or rigorously stirred in any possible way.
- - Cow urine: It should not have any turbidity in appearance or strong pungent smell. Foaming is observed when it is mixed with other contents. It ensures the fresh and qualitative aspect of cow urine. In absence of fresh cow urine, its extract (gomutraarka) is used after diluting it in 1:2 or 1:3 ratio with lukewarm water.
B) Administration of basti to the patient:
- - Vaitaranabasti should be administered at evening or in morning hours of day because during that time of a day pitta predominance is at its lower range or should say tikshnaguna effect is at its lowest peak
- - Per rectal examination should be done before administration to check any anorectal disease like pile mass, sentinel tag, inflammation, fissure etc.Vaitaranabastiis contraindicated in such conditions.
C) Clinical indications and contraindications of vaitarana basti: The classical references of indications include shoola,anaha, amavata. Following table shows clinical conditions in which vaitarana basti can be useful as well as contraindications.
| Classical References | Current clinical correlations |
|---|---|
| Shoola (pain) | Vatashonita -Kaphaanubandha, amavastha of Sandhivata. Rhematoid Arthritis, Osteoarthritis, Gout Arthritis, Ankylosing Spondylitis, Systemic Lupus Erythematous, Avascular Necrosis. |
| Anaha (flatulence) | Vaitaranabastiis contraindicated in flatulence originated due to any space occupying lesion, Ileitis, Colitis, Pancreatitis, Hepatitis, Chronic Liver Disease, High Grade Fever, Crohn’s Disease, Ulcerative Colitis. |
| Amavata | Rheumatoid Arthritis,Osteoarthritis,Gout Arthritis,Ankylosing Spondylitis, Systemic Lupus Erythematous,Intervertebral Disc Prolapse,GreevagataVata,JanugataVata,Katigraha,Katishoola,Frozen Shoulder. |
Other contraindications:
- Anal diseases
- Skin diseases
- Blood disorders
- Pitta prakriti
Current research works
- It is noticed that relief in sign and symptoms were found in patients when treated with vaitaranabasti and VatariGuggulu. Thus, it can be said that vaitaranabastiworks as a curative as well as purifying measure. Proper diet restrictions as per prakriti of a patient must be followed. This will provide a better and healthy life to Amavata patients.[12]
- The study reveals that a patient has got significant result infunctional score and swelling. Patients had got very significant result in morning stiffness, pain, tenderness & grip. Since amavata is an autoimmune disease patients may require second course of the same pattern.[13]
- It is noticed that relief in signs and symptoms of amavata was found in both groups. Comparatively, Valuka sweda with Vaitarana Basti group showed better results.[14]
- The clinical assessment of results proves the efficacy of vaitarana basti with moderate improvement in symptoms.[15]
- Vaitarana basti can be used in the disease in which niruha basti is indicated and which are caused due to Ama; vaitarana basti have significant result in sandhigata vata (upastambhita).[16]
- Vaitaranabasti is an effective treatment in the management of Amavata & it shows long lasting result. vaitarana basti can be administered without prior snehapana, swedana or virechana.[17]
- Vaitarana basti and virechana karma is an effective treatment in the management of amavata. Proper line of treatment gives better result in Ayurveda.[18]
- In this single center, randomized, open clinical study total 30 patients diagnosed with amavata were selected. In one group Alambushadi Ghana Vati (each 500 mg) two tablets thrice a day was given and in second group Alambushadi Ghana vati with Vaitarana basti on alternate day (15 days) was administered. The result shows that excellent relief in 20% patients, significant relief in 60% patients, moderate relief in 13.33% patients, whereas mild relief in 6.66% patients. Research study concluded that comparing the effect of two therapies (Alambushadi ghana vati along with vaitarana basti) provided better relief than (Alambushadi Ghana Vati alone) in most of the signs and symptoms of the disease at significant level.[19]
- Vaitarana basti is one of the most effective and economical basti which can be administered in a wide range of diseases.[20]
- The majority of the content drugs of vaitarana basti are having laghu, ruksha, ushnaand tikshna properties which pacifies vata kapha dosha. Vaitarana basti shows significant effect in ama, shula and shotha avastha.[21]
- Pharmacognostical studies shows that authentic drugs were used for preparation of the formulation and the physiochemical analysis indicates that the formulation meets all the qualitative standards. Current literature review indicates that characterization parameters of vaitarana basti are not reported anywhere so the parameters discussed here may be used as identification tools for the quality assessment of vaitarana basti.[22]
Vaitarana basti is primarily depicted in the following texts:
B. Chakrapanidutta. Chakradutta with BhavarthaSandipaniHindiVyakhya. Varanasi; Chaukambha Sanskrit Sansthan; 1961.
C. Vangasena-Vangasena Samhita, Vol.2. Second edition. By Nirmal Saxena. Varanasi: Chaukambha Sanskrit Sansthan; 2001.
D. Vrndhamadhav-Sidhayogah, Part 2. First edition. By Dr. Premvati Tiwari & Dr. Asha Kumari. Varanasi: Chaukambha Sanskrit Sansthan; 2006.
References
- ↑ Vrindha. Vrindha madhava/sidhayogah Part 2. First edition. ByDr. Premvati Tiwari & Dr. Asha Kumari.Varanasi; ChaukambhaSanskrit Sansthan; 2006.p.938.
- ↑ Vagbhata. Ashtanga Hridaya. With Commentaries SarvangaSundari of Arunadatta and Ayurvedarasayana of Hemadri.Varanasi; Chaukambha Sanskrit Sansthan; 2012. p.269. [A.H.SU19/45].
- ↑ Anonymous. The Ayurvedic Pharmacopoeia of India, Part-1, Vol-6. PgNo.206/207/224/225 part1 vol-3 PgNo.16/17.
- ↑ Sarker A, Ghosh A, Sarker K, Basu DJ, Sen DJ. Halite; the Rock Salt: enormous health benefits. World Journal of Pharmaceutical Research.2016;5(12):407-16.
- ↑ Caluwe ED, Halamova K, Damme PV. Tamarind (Tamarindus indica L.): A Review of Traditional Uses, Phytochemistry and Pharmacology. In: Juliani H, et al. African Natural Plant Products: New Discoveries and Challenges in Chemistry andQuality. Washington, DC: ACS Symposium Series, American Chemical Society; 2010. p. 85-110.
- ↑ Pandey G. DravyagunaVijnan, Part-1. Varanasi: Krishna DasAcademy; 1998. p.119-128.
- ↑ Kuru P. Tamarindus indica and its health-related effects. Asian Pacific Journal of Tropical Biomedicine. 2104; 4(9):676-681.
- ↑ Srivastav P. Verma AK, Walia R, Rehena P, Singh AK. Europeanjournal of Pharmaceutical and Medical Research. 2016.3 (3):198-202.
- ↑ Nadkarni KM, Nadkarni AK. Indian Materia Medica. 3rd edition. Bombay; Popular Prakashan; 1976.
- ↑ Vagbhata. Ashtanga Hridaya. With Commentaries SarvangaSundari of Arunadatta and Ayurvedarasayana of Hemadri.Varanasi; Chaukambha Sanskrit Sansthan; 2012. p.83[A.h.Sus.5/82].
- ↑ Randhwa GL, Sharma R. Chemotherapeutic potential of cow urine: A review. Journal of Intercultural Ethnopharmacology. 2015;4(2):180-6.
- ↑ Virmani M, Kaushik AK, Virmani G. A Clinical Study Of Vaitarana Vasti andVatariGuggulu In Aamvata (Rheumatoid Arthritis). PARIPEX Indian journal of Research 2017;6(11):114-5.
- ↑ Wadhava RS, Ghore JK. Efficacy of VaitaranaVasti and SimhanadGuggulu in Amavata. International journal of Applied Ayurveda Research 2015;II(II):230-5.
- ↑ Pooja BA, Bhatted SK, Bhojani M. Role of ValukaSweda and Vaitarana Basti in the management of Amavata (Rheumatoid Arthritis). Int J Res Ayurveda Pharm. 2013;4(5):712-4.
- ↑ Mishra SC. A piloting study on GodugdhayuktaVaitarana Basti in Vataj Gridhrasi (Sciatica). Intenational Journal of Ayurveda and Pharmaceutical Chemistry 2014;I(1). Available from: http://ijapc.com/vol1/4.pdf
- ↑ Chaudhari T, Karande L, Gahukar D. Evaluation of the effect of Vaitarana Basti in Sandhigata Vata (Upastambhit) w.s.r to inflammatory arthritis. AYUSHDHARA 2016;3(5):853-6.
- ↑ Wanole RM, Chothe DS. Vaitarana Basti in – Amavata A pilot study. Europian Journal of Pharmaceutical and Medical Research 2016;3(11):379-82.
- ↑ Medi S, Wange D. Efficacy of Vaitaran Basti and Virechana Karma along with Shaman Chikitsa in the management of Amavata (Rheumatoid Arthritis) –Case Study. World Journal of Pharmaceutical Research 2017;6(14):478-87.
- ↑ Sasane P, Saroj UR, Joshi RK. Clinical evaluation of efficacy of Alambushadi Ghana Vati and Vaitarana Basti in the management of Amavata with special reference to rheumatoid arthritis.Ayu 2016;37(2):105-12.
- ↑ Aswani PS, Ratha KK, Dighe DP, Rao MM, Remya V. VaitaranaVasti - A Conceptual Study. Research Journal of Pharmacology and Pharmacodynamics.2018;10(1):45-50. doi: 10.5958/2321-5836.2018.00008.3 .
- ↑ Mukherjee A, Dwivedi OP, Dr. Jain J, Khuje SMR. Efficacy of Vaitarana Basti with respective to Ayurveda, Journal of Drug Delivery and Therapeutics. 2018;8(6-s):246-50 doi:http://dx.doi.org/10.22270/jddt.v8i6-s.2122.
- ↑ Pravin Kumar KS, Thakar AB, Harisha CR, Shukla VJ. Pharmacognostical And Preliminary Physicochemical Evaluation OfVaitarana Basti. 2020;7(3):343-6.