Difference between revisions of "Kidney diseases"
| Line 91: | Line 91: | ||
'''Auto-immune diseases:''' Lupus, systemic sclerosis | '''Auto-immune diseases:''' Lupus, systemic sclerosis | ||
| − | In children: Congenital anomalies of kidney and urinary tract(49.1%), steroid resistant nephrotic syndrome(10.4%), chronic glomerulonephritis, e.g., lupus nephritis, Alport syndrome (8.1 %), renal ciliopathies(5.3%).<ref>Francesca Becherucci,Rosa Maria Roperto,MarcoMaterassiand Paola Romagnani- Chronic kidney disease in children- Clinical Kidney Journal 2016 Aug; 9(4): 583–591.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4957724/</ref> | + | In children: Congenital anomalies of kidney and urinary tract(49.1%), steroid resistant nephrotic syndrome(10.4%), chronic glomerulonephritis, e.g., lupus nephritis, Alport syndrome (8.1%), renal ciliopathies(5.3%).<ref>Francesca Becherucci,Rosa Maria Roperto,MarcoMaterassiand Paola Romagnani- Chronic kidney disease in children- Clinical Kidney Journal 2016 Aug; 9(4): 583–591.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4957724/</ref> |
Some of the less common causes are thrombotic microangiopathies (especially, atypical haemolytic uraemic syndrome), nephrolithiasis/nephrocalcinosis, infectious and interstitial diseases. | Some of the less common causes are thrombotic microangiopathies (especially, atypical haemolytic uraemic syndrome), nephrolithiasis/nephrocalcinosis, infectious and interstitial diseases. | ||
Revision as of 13:07, 11 January 2022
| Section/Chapter/topic | Concepts and Contemporary Practices -Nidana Chikitsa / Vyadhi / Kidney diseases |
|---|---|
| Author | Prof. Gupta S. N. 1 |
| Reviewer | Basisht G.2 |
| Editors | Deole Y.S.2, Aneesh E.G.2, Basisht G. 2 |
| Affiliations |
1 Distinguished Professor, Post Graduate Department of Kayachikitsa in J.S Ayurveda College, Nadiad, Gujarat, India 2Charak Samhita Research, Training and Development Centre, I.T.& R.A., Jamnagar, Gujarat, India |
| Correspondence email: | carakasamhita@gmail.com |
| Date of first publication: | January 10, 2022 |
| DOI | Under process |
This article is based on a lecture delivered by Prof. (Dr.) S.N. Gupta, Distinguished Professor, Post Graduate Department of Kayachikitsa in J.S Ayurveda College, Nadiad, Gujarat, India, in Prof. M. S. Baghel Memorial Lecture Series on December 09, 2021.
Incidence of chronic kidney disease
Chronic kidney disease (C.K.D.) is a big challenge to the medical fraternity. About 9.1 % of world population is suffering from CKD.[1] Kidney disorders are the 12th leading cause of death worldwide with an annual death rate of 15.7 per 100000. In India, it is the 8th leading cause of death.[2] Currently, over 2 million people worldwide need dialysis or a kidney transplant for life. However, this number represents only 10% of the people who need these kinds of treatments to save their life. The majority of these patients belong to countries like United States, Japan, Germany, Brazil and Italy. In about 100 developing countries making 50% of world population, only 20% of patients receive these facilities.[3] So, the accessibility and affordability of advanced conventional treatment facilities like dialysis and kidney transplantation are very poor especially in developing countries. Therefore, the need of systems like Ayurveda is high on rise.
Ayurveda treatment can provide relief in a patient of chronic kidney disease in either of the following three ways :
- Reduction in the frequency of dialysis (in patients who are already undergoing dialysis)
- Postponement of need of renal replacement therapy (RRT), if the patient has not yet started dialysis or not yet planned for kidney transplant
- Normal comfortable life without RRT (in less severe cases)
Ayurvedic perspective of chronic kidney disease
Chronic kidney disease (CKD) can be termed as “Jeerna or Pravruddha Vrikkadosha” in Sanskrit language. A disease condition with similar clinical features is described in Charak Samhita in Chhardi Chikitsa. [Cha. Sa. Chikitsa Sthana 20/16-17] It is a fatal condition. When the morbid vata occludes the channels carrying faeces, sweat, urine and body fluids and moves upwards, then the morbid matter from the koshtha (gastrointestinal tract), gets incited to cause vomiting. It has the following characteristics:
- Vomitus having color and odor of the faeces and urine;
- Persistent thirst, dyspnoea hiccup and pain
- Vomiting of foul smelling or dushta (putrid material); and
- Bouts of vomiting ejected with great force.
Such a patient succumbs to death quickly. This shows a clear picture of a uremic patient with vomiting, uremic smell, thirst, breathlessness and hiccup. Management of this condition is not described which shows that in that period management of this condition was not available.
Concepts of kidney and formation of urine
There are no direct references in Ayurvedic classics regarding the role of kidneys in the process of formation of urine. The word pakwashaya (colon) is mentioned as the site of formation of urine. It should not be considered in anatomical or physiological aspects of conventional medicine. Ayurvedic texts emphasize more on therapeutic relevance of the organs. The description may not always match with modern views. This concept has a very good therapeutic utility. The drugs and therapies having action on colon (pakwashaya) are successfully used for promoting proper formation of urine from its original site (kidney).
Word vrikka is found in Rigveda but not as an organ but as a medicinal plant. According to Bhashya the word vrikka means ‘averter of diseases’. Thus, in similar manner we may understand the vrikka as organ also. [Rigveda 1/187/10]
Similarly, the word “vrukka” used for denoting kidneys indicate that it has the capacity of healing itself. This self-healing power of vrukka (kidney) shall be explored and promoted by Ayurvedic treatment.
Chronic renal failure
By definition, chronic renal failure (C.R.F.) is an irreversible deterioration in the renal function, classically develops over a period of years with a decline in glomerular filtration rate (GFR) below 60 ml/min/1.73 m2 of body surface area for more than 3 months. However, clinically, the deterioration in renal function is found to be reversible to some extent. It is certainly not a completely curable disease. When the GFR becomes <15 ml/min/1.73 m2 of body surface area, it is known as end stage renal disease (ESRD).
Pathogenesis of ESRD
When any pathological changes occur in kidney, initially there is hyperfiltration leading to minor damages to the kidney. Because of this hyperfiltration, there is over burden to the remaining healthy nephrons to compensate it. This causes further damage in the healthy nephrons and progressive dysfunction ultimately leading to ESRD. Initially it will be evidenced by biochemical abnormalities, but gradually it leads to excretory, metabolic and endocrinal deficiencies related to the functions of kidney.
Etiological factors
Congenital causes: Polycystic kidney, congenital hypoplasia
Vascular causes: Arteriosclerosis, renal artery stenosis, diabetic nephropathy, haemolytic uremic syndrome, vasculitis
Glomerular disease: Various types of glomerulonephritis (primary glomerular disease such as focal segmental glomerulosclerosis and IgA nephropathy)
Intestinal diseases: Chronic pyelonephritis, vesico-ureteric reflux, tuberculosis, calcinosis, analgesic nephropathy
Obstructive uropathy: Calculus, prostatic hypertrophy, pelvic tumours
Auto-immune diseases: Lupus, systemic sclerosis
In children: Congenital anomalies of kidney and urinary tract(49.1%), steroid resistant nephrotic syndrome(10.4%), chronic glomerulonephritis, e.g., lupus nephritis, Alport syndrome (8.1%), renal ciliopathies(5.3%).[4]
Some of the less common causes are thrombotic microangiopathies (especially, atypical haemolytic uraemic syndrome), nephrolithiasis/nephrocalcinosis, infectious and interstitial diseases.
Etiopathogenesis as per Ayurveda
The etiological factors can be understood and categorized in the following manner.
- Genetic abnormalities (bija dosha)
- Suppression of natural urges, especially those related to the action of apanavayu (type of vata dosha responsible for excretory functions).
- Injury to vital organ (marmabhighata): Especially on three major vital organs (shira, hrudaya, basti)
- Faulty dietary habits (vishamashana)
- Diseases of urinary system (mutravahasrotas) e.g. mutrakricchra, mutraghata, ashmari, arbuda, granthi, prameha (especially madhumeha)
- Auto immune factors (balabhramsha)
- Accumulation of intermediate products produced during digestion, metabolism and transformation (amasanchiti)
- Chronic debilitating illnesses (jeernajwara)
- Unknown causes (daiva)
Dosha- dhatu involvement in pathogenesis
In this condition, there is involvement of all the three dosha with predominance of vata and kapha dosha. The bodily components that get vitiated in initial stage are urine (mutra), body fluids (rasa, udaka, sweda, rakta) and blood vessels (sira). In later stages all the tissue components (dhatu and upadhatu) may get involved. Clinical conditions related to tendons (snayu), muscles tissue (mamsa), bones (asthi) and reproductive components (shukra) are often observed related to kidney diseases.
Srotas
In initial stage, channels(srotas) like urinary (mutravaha), body water (udakavaha), sweat (swedavaha), body fluids (rasavaha) and blood (raktavahasrotas) are involved. But gradually it advances into a multi system disorder.
The pathological changes happening in the channels of urine(mutravahasrotas) in patients of chronic kidney diseases can be interpreted in terms of guna (inherent qualities). Excessive increase in characteristics like roughness (kharatwa), heaviness (gaurava), hardness (kathinya) and dryness (raukshya) leads to the structural damages in advanced stage.
The functions of agni are deteriorated at every level. Accumulation of intermediate products formed during digestion and metabolism (ama) is seen in every stage. The origin of all these pathological changes is colon (pakwashaya). The disease with initial involvement of middle pathway (madhyamarogamarga) progress to all the three disease pathways (rogamarga). This leads to poor prognosis.
Principles of Management
- First and most important step is avoiding causative factors (nidanaparivarjana) with treatment of underlying diseases.
- Repair of the damage at the site of origin for disease i.e., kidneys
- Establishing the normal state of channels of urine, body fluids and sweat by supporting the excretory functions and maintenance of fluid and electrolyte balance.
- Nourishment of the supportive tissues (dhatu poshana) especially rasa, rakta, mamsa and asthi dhatu. This includes correction of anaemia, myopathy, neuropathy, osteodystrophy etc.
- Management of associated problems such as cardiovascular disorders, hypertension etc.
- Psychotherapy (sattvavajayachikitsa) and spiritual therapy (daivavyapashrayachikitsa)
I. Avoiding the cause (nidanaparivarjana)
With the advice for avoiding the causative factors like dietary, life style modifications etc. the underlying disease conditions should be addressed first.
In cases of polycystic kidneys, manage the condition with suitable medicines like Kanchanaraguggulu, Varunadikwatha etc. For example, in case of hypertension, use of antihypertensive drugs to control blood pressure and overload on kidneys. In case of diabetic nephropathy, treatment for diabetes should be done first.
II. Repairing the damage at kidneys (origin of disease)
Herbs having rasayana (rejuvenating) activities on urinary system (mutravahasrotas) should be used. Crataeva religeosa (varuna), Boerrhavia diffusa (punarnava), Tribulus terrestris (gokshura), and Phyllanthus niruri (bhumyamalaki) show potent rejuvenating activities on urinary system. The compound preparation called “Chyavanaprasha”, other preparations like Jivitapradavati [Bheshaj Samhita],[5] shilajatwadivati etc. with rasayana drugs like black bitumen (shilajatu) and Commiphora wightii (guggulu) are found very effective for this purpose.
III. Establishing the normal state of srotas (mutravaha, udakavaha and swedavaha)
In order to support the excretory functions and maintenance of fluid and electrolyte balance, the therapeutic procedure called ‘basti’ is found highly effective. The decoction enema (niruha basti) with punarnavadi kwatha, and unctuous enema (anuvasana basti) with gokshuradi taila, the drug Boerrhavia diffusa (punarnava) in a palatable and convenient form 3-5 g twice a day is advisable.
Fluid intake should be regulated according to urine output. Excessive fluid intake is not advisable as it causes extra burden to the nephrons. However dehydration by restriction of fluids shall be prevented.
The status of important electrolytes like sodium and potassium should be considered. In cases of hypernatremia and associated cardiac failure, salt should be restricted. Rock salt (saindhava lavana) is advisable if needed. In cases of hyperkalaemia, intake of fruits and vegetables should be restricted. In case of hypokalaemia, intake of fruits and coconut water is useful.
IV. Nourishment ofdhatu (body constituents)
For correction of anaemia, Chyavanaprasha or any iron containing preparations are effective. Role of erythropoietin shall be considered here. If only the excretory function of kidney is impaired and endocrinal functions are proper, then erythropoietin supplementation is not needed. In case of deficiency of erythropoietin only, it should be supplemented. Fruits of prickly pear, beetroot are natural supplements having similar action to erythropoietin. These are used for promoting blood tissue (rakta dhatu).
For managing myopathy and neuropathy, a very effective therapeutic measure is massage (abhyanga) with medicated oils. This pacifies aggravated vata dosha. For osteodystrophy, Shankhabhasma, compounds of mukta (pearl) and pravala (coral) are used. They are good natural source of calcium and also help in managing hyperacidity. Mukta is an antidepressant too.
V. Management of associated conditions
In cases of hypertension, Triphala guggulu 1gm three times a day along with powder of Terminalia arjuna (3g) is effective. The powder of Rauwolfia serpentina (sarpagandha) 500mg-1gm can also be given to control hypertension. Symptomatic treatments are given in cases of nausea, vomiting, hiccup etc.
VI. Psychotherapy
Proper counselling of the patients, giving positive outlook and assurance comes under sattvavajaya chikitsa. This has a great role in such conditions.
Treatment protocol
Purification therapies (shodhana chikitsa)
In mild cases (creatinine <3mg%), mild therapeutic purgation (virechana) is advised after oleation (snehana) with gokshuradi ghrita. Then medicated enema (basti) with punarnavadi kwatha and gokshuradi taila is given.
If auto immune factors are involved, use of Piper longum (pippali) in the specific ascending and descending doses (vardhamana pippali) is recommended before virechana procedure.
Pacification therapies (shamana chikitsa)
Following medications are found effective in the management of kidney diseases.
- Gokshuradi guggulu-1g, three times a day, after food with warm water
- Varunadi kwatha - 40ml, two times a day
- Rasayana Churna [a combination of Tribulus terrestris (gokshura), Embilica officinalis (amalaka) and Tinospora cordifolia (guduchi)], 3g, three times a day with water
- Shvadamshtra Rasayana (powder of Tribulus terrestris (gokshura) triturated 7 times in the decoction of the same drug) 1g, three times a day
- Powder of Phyllanthus niruri (bhumyamalaki)– 3g, three times a day, after food, with water.
- Shilajatwadi vati-750mg, three times with water.
Dietary protocol
Breakfast: Chyavanaprashaavaleha 20g with 300ml boiled cow’s milk.
Lunch: Boiled green gram, green gram soup, boiled vegetables, rice. Fresh and mild spices are added.
Supper: Green gram soup, beans soup, rice, boiled vegetables with mild to moderate spices.
Others: Fruits (only papaya, grapes, sweet apple, figs and dates), pop rice.
An extra 100 ml of boiled milk (cow’s) is also advisable during day time, if the patient feels hungry.
Food items to be avoided:
- All other flour items like wheat, millet, corn etc.
- Bakery items, junk food, fermented items
- All oils except sesame oil
- Salts, sour substances
- Chilies, deep fried items
- Milk products except cow’s milk and ghee are to be avoided.
Lifestyle factors
Excessive physical and mental stress, day time sleep and night vigil are also restricted.
Current research
A clinical study of 100 patients of chronic renal failure (other than diabetic nephropathy) to study effect of ayurveda therapy was conducted. Decoction enema (niruha basti) with punarnavadi kwatha daily and oral administration of gokshuradi guggulu, rasayana churna and varunadi kwatha as per the protocol were prescribed for a period of one month. In this study, statistically significant results were obtained in levels of serum creatinine, blood urea and albumin in urine along with considerable relief in signs and symptoms.[6]
Another study was conducted in 130 patients of diabetic nephropathy treated with oral administration of gokshuradi guggulu, bhumyamalaki, vasa and shilajatvadivati for 2 months. The data showed highly significant reduction in serum creatinine, blood urea and urinary excretion of albumin.[7]
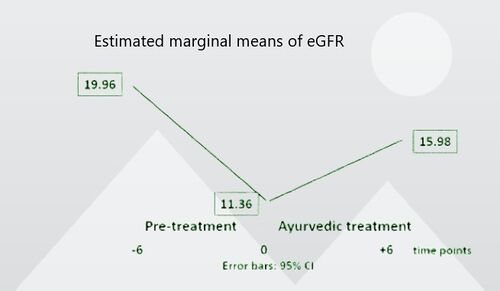
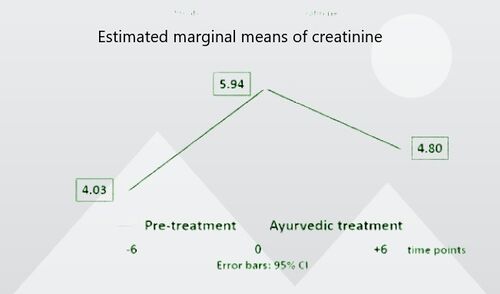
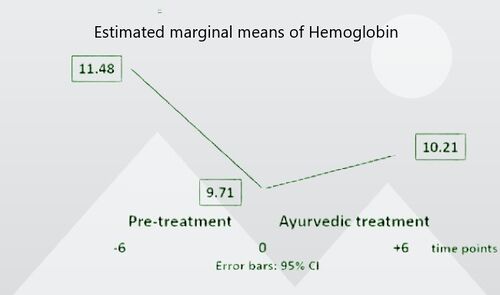
In a study, sixty-four non-dialysis CRF patients with stage IV or V at base line and having record of laboratory investigations of the preceding 6 months were studied. The treatment protocol included enemas (niruha-basti) containing 40 ml punarnavadi kwatha daily one hour before lunch for one month. Oral medications like gokshuradi guggulu, varunadi kwatha, rasayana churna, bhumyamalaki, shilajatwadivati, and chyavanaprasha were given for six months. Renal function tests (RFTs) were evaluated at various time points, i.e 6 months before baseline (TP -6), at baseline (TP 0), and after completion of 6 months of treatment (TP +6). After six months of Ayurvedic treatment, statistically and clinically significant improvements of eGFR, serum creatinine, blood urea, and hemoglobin and a significant shift to better CRF stages were observed in this study.[8]
Possible modes of action
- Mental positivity
- Deceleration of disease process
- Reversal of pathology in mild affected units
- Adaptation
- Compensation by intact nephrons/by other organs
Clinical Studies on effect of Ayurvedic treatment on dialysis dependent patients are under progress.
Send us your suggestions and feedback on this page.
References
- ↑ Carney, E.F. The impact of chronic kidney disease on global health. Nat Rev Nephrol 16, 251 (2020). https://doi.org/10.1038/s41581-020-0268-7
- ↑ Jha V, Garcia-Garcia G, Iseki K, Li Z, Naicker S, Plattner B, Saran R, Wang AY, Yang CW. Chronic kidney disease: global dimension and perspectives. Lancet. 2013 Jul 20;382(9888):260-72. doi: 10.1016/S0140-6736(13)60687-X. Epub 2013 May 31. Erratum in: Lancet. 2013 Jul 20;382(9888):208. PMID: 23727169.
- ↑ Couser WG, Remuzzi G, Mendis S, Tonelli M. The contribution of chronic kidney disease to the global burden of major noncommunicable diseases. Kidney Int. 2011 Dec;80(12):1258-70. doi: 10.1038/ki.2011.368. Epub 2011 Oct 12. PMID: 21993585.
- ↑ Francesca Becherucci,Rosa Maria Roperto,MarcoMaterassiand Paola Romagnani- Chronic kidney disease in children- Clinical Kidney Journal 2016 Aug; 9(4): 583–591.https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4957724/
- ↑ Bheshajasamhita( Ayurvedic pharmacopeia)Edited by Gujarat state bheshaja samiti 1st edition, Ministry of health, Gujarat State; 1966 P 468-9
- ↑ Patel MV, Gupta SN, Patel NG. Effects of Ayurvedic treatment on 100 patients of chronic renal failure (other than diabetic nephropathy). Ayu. 2011;32(4):483-486. doi:10.4103/0974-8520.96120
- ↑ Patel K, Gupta SN, Shah N. Effect of Ayurvedic management in 130 patients of diabetic nephropathy. Ayu. 2011;32(1):55-58. doi:10.4103/0974-8520.85727
- ↑ Patel M, Patel M, Patel K, Wischnewsky M, Stapelfeldt E, Kessler CS, Gupta SN. Deceleration of Disease Progress Through Ayurvedic Treatment in Nondialysis Stages IV-V Patients with Chronic Renal Failure: A Quasi-Experimental Clinical Pilot Study with One Group Pre- and Postdesign and Two Premeasurements. J Altern Complement Med. 2020 May;26(5):384-391. doi: 10.1089/acm.2019.0419. Epub 2020 Mar 30. PMID: 32223566.