Cardiac diseases
| Section/Chapter/topic | Concepts and Contemporary Practices -Nidana Chikitsa / Vyadhi / Cardiac diseases |
|---|---|
| Author | Dr. Sane Rohit 1 |
| Reviewer | Basisht G.2 |
| Editors | Deole Y.S.2, Aneesh E.G.2, Basisht G. 2 |
| Affiliations |
1 M.D. & C.E.O. at Madhavbaug, Vaidya Sane Ayurvedic Labs Pvt. Ltd. Thane, Maharashtra, India 2Charak Samhita Research, Training and Development Centre, I.T.& R.A., Jamnagar, Gujarat, India |
| Correspondence email: | carakasamhita@gmail.com |
| Date of first publication: | June 26, 2021 |
| DOI | Under process |
Updates on management of cardiac diseases through Ayurveda
(This article is based on lecture delivered by Dr. Rohit Sane in Prof.M.S.Baghel Memorial Lecture Series on June 09, 2021.)
The major chronic diseases prevailing in India are cardiovascular disorders (CVD), diabetes, hypertension, obesity and dyslipidemia. Mortality due to cardiovascular disease is increasing substantially. In the year 1990, the mortality rate due to CVD in India was 15.2, which increased to 28.1 in 2016.[1] Despite the advancements in modern medicine, especially in treating CVD like angioplasty, bypass surgery, etc., the disease burden is increasing. Ayurveda can play a significant role in treating CVD as a lifestyle disorder and a non-communicable disorder.
The risk factors of CVD are diabetes, hypertension, and obesity. The burden of these lifestyle disorders is also high on the rise. As per the data available, 9.7% of the adult population in India has Diabetes.[2] Hypertension is present in 25% of urban and 10% of rural subjects in India. Stage I hypertension carries significant cardiovascular risk.[3] Therefore, it is essential to treat these comorbid conditions while treating CVD.
Importance of animal trials
In Ayurvedic classical texts, different treatment techniques and different drugs are mentioned for the treatment of heart disorders. This must be reproved per the current knowledge. Animal trials are necessary to understand the mode of action of the drug along with re-establishing its efficacy.
Antihypertensive herbs
Common Ayurvedic herbs used in the treatment of hypertension and their mechanism of action is shown in Table 1 below.
| Herb | Latin Name | Mechanism of action |
|---|---|---|
| Bramhi | Bacopa monnieri | Calcium channel antagonist |
| Shunthi | Zingiber officinale | Calcium channel antagonist |
| Vacha | Acorus calamus | ACE inhibitor |
| Bibhitaki | Terminalia bellirica | ACE inhibitor |
| Pippali | Piper longum | ACE inhibitor |
| Kalaajaji | Nigella sativa | Diuretic |
| Punarnava | Boerhaviadiffusa | Diuretic |
Since Bramhi and Shunthi are calcium channel antagonists they can be used for patients with systolic hypertension. Vacha, Bibhitaki and Pippali can be used in diastolic hypertension as they are ACE inhibitors. Kalaajaji and Punarnava are excellent diuretics to be used very effectively in the early phase of hypertension.
Anti-diabeti cherbs
Some of the Ayurvedic herbs used in diabetes management and their mechanism of action are shown in Table 2.
| Herb | Latin Name | Mechanism of action |
|---|---|---|
| Daruharidra | Berberis aristata | Hypolipidemic, insulin resistance |
| Amalaki | Phyllanthus emblica | Beta cell-protective & beta cell regenerative |
| Haridra | Curcuma longa | Hypolipidemic & Beta cell protective |
| Vishanika /Gudmar* | Gymnema sylvestre | Insulin secretogogues |
| Banaba/ Jarul | Lagerstroemia speciosa | Insulin secretogogues |
*Gudmar also has the capacity to produce a coat over the intestine so that the carbohydrate absorption through the gut gets reduced.
Herbs for management of coronary artery disease
The coronary artery disease (CAD) is caused due to atherosclerosis. The deposition of cholesterol and fatty tissue form plaque in the endothelium of coronary arteries. This causes clogging or damage to the artery and hamper blood circulation to myocardium. Ayurvedic herbs are described as hridya (beneficial for heart) in [Charak Samhita Sutra Sthana 4/10]. Some of the researched herbs used in the management of coronary artery disease (CAD) and their mechanism of action are shown in Table 3.
| Herb | Latin Name | Mechanism of action |
|---|---|---|
| Vrikshamla | Garcinia indica | Anti inflammatory, Hypolipidemic |
| Matulunga | Citrus medica | Anti inflammatory, Hypolipidemic |
| Amlavetasa | Rheum emodii | Anti inflammatory, Hypolipidemic |
| Pushkaramula | Inula racemosa | Anti inflammatory, Hypolipidemic |
Experimental studies on hridya herbs
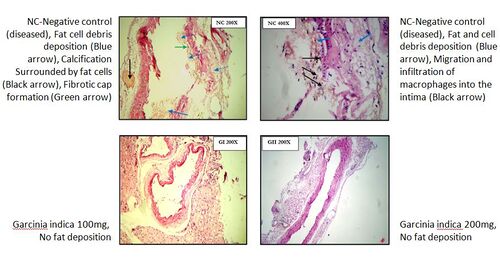
Various experimental studies are conducted to study the effect of herbs in reducing atherosclerosis. The animals were first fed with high fat, high cholesterol diet. As a result, the endothelium of vessels gets deposited with fatty tissues (atherosclerosis), which is considered as the primary cause for blockages. Then the same animals were fed with CAD reversal herbs like Garcinia indica (Vrikshamla) for six weeks. Garcinia treatment protected the endothelium from atherosclerosis.The endothelium becomes intact without any fatty tissue deposition.[4]
Sampurna Hridaya Shuddhikaran (SHS) therapy
A treatment protocol named “Sampurna Hriday Shuddhikaran” (Total Purification of Heart) is developed by an amalgamation of ayurvedic and modern medical knowledge. It is an interventional health model to improve the quality of life in chronic heart failure patients.
A single session of sampurna hridaya shuddhikaran (SHS) is of 90 minutes duration. A session of SHS includes four main procedures.
- Oleation (snehana): It includes whole-body massage in the form of strokes from the periphery towards the heart. Sesame oil processed with Terminalia arjuna, Vitex nigundo and Dashamula (group of 10 herbs) is used for massage.
- Fomentation (swedana): Fomentation is given by keeping the patient inside a wooden chamber. The vapor is produced out of decoction prepared with Dashamula.
- Dripping decoction on chest/cardiac region (Hrudaydhara): The warm decoction prepared with Dashamula is dripped in a continuous stream from a height of 7-8 cm to the medial mediastinum region.
- Therapeutic enema (basti): Decoction enema prepared with Terminalia arjuna, Acorus calamus, and Boerhavia diffusa is administered.[5]
Effects of SHS therapy
Improvement in quality of life and VO2 max
VO2max is the measurement of the volume of oxygen that the body can utilize during physical exertion. In chronic heart failure, the person feels breathless after walking for a certain distance. A total of 692 chronic heart failure patients were recruited in a trial to assess the efficacy of SHS therapy. At the end of this therapy, the patients were assessed for quality of life. It is found that the quality of life improved substantially, and VO2 max was also improved.[6]
Improvement in exercise tolerance
The American heart association prescribes the six-minute walk test (6MWT) for chronic heart failure (CHF) patients. Average persons can walk 350m in 6 minutes. However, patients with CHF are unable to cover that distance in 6 minutes. In a study on 200 patients of CHF, the SHS therapy with Madhavbaug Cardiac Rehabilitation Centre (MCRC) protocol on stress test showed improvement in cardiac effort tolerance of 132.1 seconds on the sixth day. The Sampurna Hridhay Shuddhikaran (SHS) model was observed very much effective in improving the exercise tolerance of Chronic Heart Failure patients. This improvement is independent of Age, Sex, and BMI of the study participants.[7]
Improvement in ejection fraction
A prospective interventional study on 133 patients was conducted to assess the efficacy of SHS on the ejection fraction. The preintervention ejection fraction (39.43) was significantly increased to 45.98 after 30 days of Sampurna Hridaya Shuddhikaran treatment. SHS showed improvements inejection fraction, myocardial thickness, and exercise tolerance.[8]
Effect of SHS with slightly modified protocols is studied in different research programs titled Heart Failure Reversal Therapy (HFRT) and Ischemia reversal program (IRP).
HFRT (Heart failure reversal therapy)
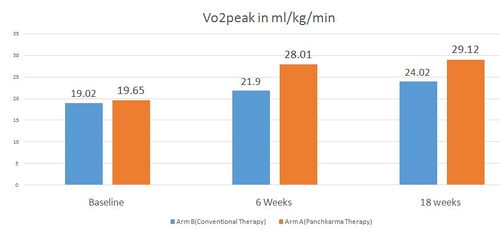
In a randomized controlled trial, one group (Arm A) received HFRT (Heart failure reversal therapy) with conventional oral medications for heart failure. The other group (Arm B) received only conventional oral medications. VO2 max in Arm B group was 19.02ml/kg/min initially. After six weeks of conventional treatment, VO2 max increased to 21.9ml/kg/min. After 18 weeks, it again raised to 24.02 ml/kg/min. The initial VO2 max in Arm A patients was 19.65 ml/kg/min, almost equal to that of Arm B. After six weeks of therapy VO2 max raised to 28.01 ml/kg/min, and after 18 weeks of therapy, it again raised to 29.12 ml/kg/min.[9] [Image 2] This shows the significant advantage of HFRT over conventional treatment in heart failure.
Efficacy in ischemic heart disease
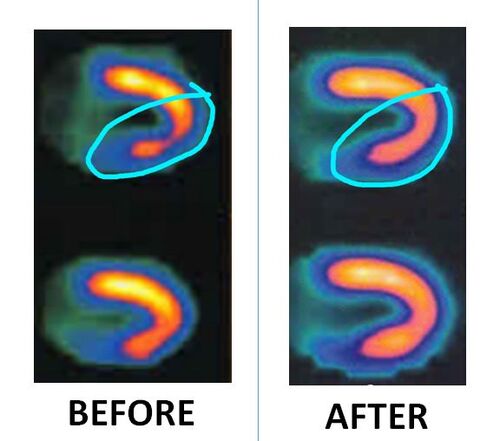
Stress Thallium test was applied to assess the reversal of ischemic changes in patients of CHF associated with myocardial ischemia. The radioactive isotope Thallium was injected into the bloodstream of cardiac patients. Gamma scanner was used to assess the circulation of thallium in the myocardium. After three months of ischemia reversal program, 30.33% of the reduction was observed in ischemia on Myocardial Perfusion through SPECT MPI.[10]
Effect on left ventricular distress
Efficacy of Heart Failure Reversal Therapy (HFRT) in reducing left ventricular distress was studied. N-terminal pro-brain natriuretic peptide (NT-proBNP) was used as a marker to assess the effect of therapy in congestive heart failure (CHF)patients.The value of NT-ProBNP increases with an increase in the severity of CHF. The study therapy, HFRT, including SHS protocol, was administered twice daily for seven days. Post-HFRT, decoction prepared with Terminalia arjuna, Acorus calamus, and Boerrhavia diffusa was administered for the next 12 weeks of follow-up. NT-proBNP levels were measured after a follow-up period of 90 days along with some other parameters like BMI, VO2peak (evaluated by cardiac stress test with modified Bruce protocol) and weight. The findings of the investigation revealed a significant reduction in NT-proBNP levels (42.46%, p = 0.009) at the end of the follow-up period. The study also yielded significant improvements in VO2peak (50.96%, p = 0.004). The overall results suggest that HFRT can possibly be explored as add-on therapy or a feasible alternative for the effective management of CHF.[11]
Mortality rate and survival
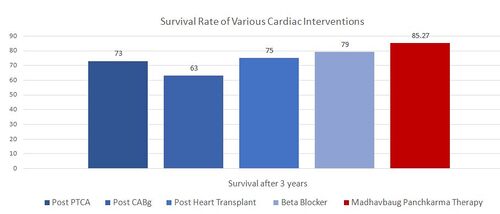
The survival rate of cardiac patients after coronary angioplasty after three years is 73%. After coronary bypass graft, the survival rate is 63%. After a heart transplant, it is 75%. Survival rate increases to 79% after taking beta-blocker drugs. The survival rate post three years of Ayurvedic panchakarma therapy at Madhavbaug rises above 85%.[12]
As per various published data, the survival rate of various cardiac interventions is shown below. [Image 4]
Conclusion
Ayurvedic treatment shows an advantageous effect in treating chronic lifestyle disorders like diabetes, hypertension, and cardiovascular disorders. Ayurvedic treatment is implemented as a first line of therapy in these disorders; then, the mortality burden can be reduced significantly.
Interactions
Q. Please share the experience in the development of collateral circulation after Ayurvedic cardiac treatment
Ans: The basic assessment for the development of collateral circulation is the stress test. For e.g.as per Bruce protocol, an increase in walking time indicates that more blood is reaching the myocardium because of the improvement in collaterals. Global longitudinal score with 2D echo with four-chamber view should be -18 and beyond. The patient with scores -10, -8 suggests the patient is ischemic. After the therapy, if the score is improving like -14, -16 etc., the collaterals are improving. But a correct identification of the cause for improvement in functions, whether it is due to collateral improvement or whether it is due to reduction in a block, is challenging to determine.
Q. Do you observe any relation between prakriti (body constitution) and its susceptibility to cardiac disorders?
Ans: Prakriti and the involvement of dosha are very much influencing the development of cardiac disorders. Typical presentations explained for different kinds of hridroga (cardiac disorders) can be seen in patients. For eg. In vataja hridroga the pain will be severe. It may be cutting, stabbing, tearing etc., in nature. In kaphaja hridrog pain will be minimal. The other symptoms like excessive salivation, heaviness in the chest etc., are more predominant. In pittaja hridroga burning in the sternum/epigastric region is the main presenting feature. The classical treatments mentioned for these individual types of cardiac disorders give an excellent result.
References
- ↑ India State-Level Disease Burden Initiative CVD Collaborators. The changing patterns of cardiovascular diseases and their risk factors in the states of India: the Global Burden of Disease Study 1990–2016.Lancet Glob Health 2018; 6: e1339–51 Available from https://www.thelancet.com/action/showPdf?pii=S2214-109X%2818%2930407-8 cited on 23/06/2021
- ↑ Akhtar SN, Dhillon P. Prevalence of diagnosed diabetes and associated risk factors: Evidence from the large-scale surveys in India. J Soc Health Diabetes [serial online] 2017 [cited 2017 Oct 15 ];5:28-36
- ↑ Gupta R. Trends in hypertension epidemiology in India. J Hum Hypertens. 2004 Feb;18(2):73-8. doi: 10.1038/sj.jhh.1001633. PMID: 14730320.
- ↑ Kim, Young-Je & Choi, Myung-Sook & Park, Yong & Kim, Sang & Lee, Mi-Kyung & Jung, Un. (2013). Garcinia Cambogia attenuates diet-induced adiposity but exacerbates hepatic collagen accumulation and inflammation. World journal of gastroenterology : WJG. 19. 4689-701. 10.3748/wjg.v19.i29.4689.
- ↑ Sane R., Rajgure V., Arute S., Parvez B. Effect of Heart Failure Reversal Therapy Program (HFRT) on Chronic Heart Failure Patients: A Retrospective Study. J. res. tradit. med. 2018;4(2):49-57
- ↑ Sane R., HanchateM.SampurnaHridayShuddhikaran: An Interventional Health Model to Improve Quality of Life in Chronic Heart Failure. The Lancet. JACC. 1st Asia Pacific Cardiovascular Summit.
- ↑ Sane R., Hanchate M. Sampurna Hriday Shuddhikaran: An Interventional Health Model to Improve Quality of Life in Chronic Heart Failure.Journal of US-China Medical Science. 2011:8 (11) (Serial No. 84), pp. 697–700.
- ↑ Sane R, Hanchate M. Effect of the Sampurna Hriday Shuddhikaran (SHS) Model in Heart Failure Patients in India: A Prospective Study. British Journal of Medicine & Medical Research, 4(1): 564-571, 2014
- ↑ Sane R, Aklujkar A, Patil A, Mandole R. Effect of heart failure reversal treatment as add-on therapy in patients with chronic heart failure: A randomized, open-label study. Indian Heart J. 2017 May-Jun;69(3):299-304. doi: 10.1016/j.ihj.2016.10.012. Epub 2016 Nov 18. PMID: 28648417; PMCID: PMC5485380.
- ↑ Rohit S, Jagdish H, Chandrakant C, Sujit N, Rahul M (2020) Ischemia Reversal Therapy as an add-on Therapy for Ischemic Heart Disease: A Pilot Study based on SPECT Myocardial Perfusion Imaging. J Cardiovasc Dis Diagn 8: 397.
- ↑ Sane R, Mandole R. To Evaluate the Efficacy of Heart Failure Reversal Therapy Using NT-Probnp Levels in Patients with Chronic Heart Failure. Cardiology and Cardiovascular Research, 2(3): 61-64, 2018. doi: 10.11648/j.ccr.20180203.13
- ↑ Sane R. Mandole R. A Retrospective cohort to study the mortality and survival rate amongst Chronic Heart Failure (CHF) patients after Ayurvedic Sampurna Hruday Shudhikaran (SHS) therapy. Paper presented in 5th Cardiology conference Philadelphia USA.