Stanya
Breast milk (stanya) is the nourishing fluid that is produced in the breasts (stana) forming the primary food for the infants. In Ayurveda, according to the branch ‘Kaumarabhritya’ includes the diseases in the neonates and infants. The diseases of newborn are caused by faulty nutrition, vitiated breast milk (dushta stanya or dosha) and presence of psychiatric conditions (graha dushti). (Su Sa. Sutra Sthana 1/8/5) There is emphasis on breast feeding explained through the concept of stanya vignyana. The knowledge or literature available on stanya is dispersed in various parts across different Samhita. This article deals with all the basic concepts related to stanya and breast milk in terms of pathology, physiology and therapeutics as mentioned in the Ayurveda Samhita and possible research perspectives in the field.
| Section/Chapter/topic | Concepts/Stanya |
|---|---|
| Authors | Bhojani M. K.1, Joglekar Aishwarya2 |
| Reviewer | Basisht G.3, |
| Editor | Deole Y.S.4 |
| Affiliations |
1 Department of Sharir Kriya, All India Institute of Ayurveda, New Delhi, India 2 Department of Samhita Siddhant, All India Institute of Ayurveda, New Delhi, India 3 Rheumatologist, Orlando, Florida, U.S.A. 4 Department of Kayachikitsa, G. J. Patel Institute of Ayurvedic Studies and Research, New Vallabh Vidyanagar, Gujarat, India |
| Correspondence emails |
meera.samhita@aiia.gov.in, carakasamhita@gmail.com |
| Publisher | Charak Samhita Research, Training and Development Centre, I.T.R.A., Jamnagar, India |
| Date of publication: | September 27, 2023 |
| DOI | 10.47468/CSNE.2023.e01.s09.152 |
Etymology
“Stanodbhavam stanyam”- the entity produced or secreted from breast (stana) is termed as ‘stanyam’. (Dalhana on Su. Sa. Nidana Sthana 10/18) Monniere Williams dictionary mentions it as that which is drawn from the breast i.e. breast milk or mothers milk.[1]
Synonyms
Naari ksheer, naari dugdha, stree dugdha, stree ksheera, ksheera, dugdha, manusha ksheera, manusha dudha, stanodbhava, yoshita stanya
Physiology of stanya according to ayurveda
Stanya is regarded as upadhatu (the minor structural components that stabilize and sustain the body) and prasada bhaga (essence or formed from nutrient part) of rasa dhatu metabolism, produced in the breast/mammary glands in females. [Cha. Sa. Chikitsa Samhita 15/17, Bhoja Samhita] Bhoja mentions stanya as not having any movement or physiological functions in body (gativivarjita) as it does not participate in further metabolic activities in the body. Sushruta mentions stanya as a product of digested food (pakwahara). [Su. Sa. Nidana Sthana 10/18] Like shukra, its presence is felt across the body. [Su. Sa. Nidana Sthana 10/19]
Kashyapa opines that stanya is produced from the rakta dhatu. [Kashyapa Samhita Rakta Gulma Adhyaya] This can be justified as the stanya is produced and expressed from the stana which consists of sira which are the upadhatu of rakta dhatu.
The metabolism of rasa- rakta dhatu form the major canvas for the understanding the stanya physiology. Like menstruation (artava), stanya is observed for limited time during the course of life of a female i.e. post delivery period or lactation period. Sushruta states that it is expressed within 3 of 4 days of child birth and its secretion continues till the stanyapanayana or weaning occurs. [Su. Sa. Shareera Sthana 10/14] [A.H. Uttar Tantra 1/14]
The development of breasts occurs after the menarche by physiologically accelerated growth of mammary glands during the pregnancy. [Su. Sa. Nidana Sthana 10/17] In the state of pregnancy, the rasa dhatu metabolism is directed towards stanya formation. [Cha. Sa. Shareer Sthana 6/23 ,Kashyap Samhita Sutrasthana 1]
As per Vagbhat, the gross amount of breast milk (stanya) present in an individual is 2 anjali[2] (approximately 200ml with 1 anjali corresponding to 135ml according to a previous study). [A.H. Shareera Sthana 3/81] According to contemporary approach average breast milk production is about 500-700ml per day.[3] It is defined to have pure white colour and becomes homologous with water when mixed. It possesses a characteristic sweet/ madhura smell when unvitiated. [Su. Sa. Shareera Sthana 8/14, Su. Sa. Nidana Sthana 10/25] Any deviation from the normal colour and consistency of stanya reflects underlying pathological condition. Sushruta has also explained the physiology of stanya.
Following factors are responsible for the appearance of breast milk in the post-natal period which also facilitates the process of labour. [Su. Sa. Nidana Sthana 10/22]-
- Apatya sparsha- Touching the child.
- Apatya darshana- Sight of the new-born.
- Apatya smarana- Thinking about the child.
- Grahanat shareerasya¬- Holding the new-born close to the mother.
Contemporary view also suggests that the hormonal and emotional factors play a key role in the breast milk physiology.[4] Thus in the conditions like decreased lactation (stanya-kshaya), counselling can prove to be more beneficial.
The main function of stanya is providing the nourishment to child as explained through the jeevana karma (promoting vitality). [Su. Sa. Sutra Sthana 15/14] The entire sustainance of the child for the first six months to one year is dependent on the stanya, which also determines the health profile of the infant. Another karma of stanya is peenatvajanana i.e. providing proper structure and nourishment to the stana or breast tissue. [Su. Sa. Sutra Sthana 15/5] Kashyapa has also emphasized the same stating the breast milk as jeevana (vitalizer), pushtikara (nourishing), vriddhikara (growth promoting), balavardhana (strengthening), ojaskara (promotinig essence part of life) [Kashyap Samhita Ksheera Vigyana Adhyaya]
Ayurveda mentions that the, expression of breast milk from the right breast at first is indicative of male progeny, while that from left breast is indicative of female progeny. [Su. Sa. Shareera Sthana 3/34, Cha. Sa. Shareera Sthana 2/24]
Breas milk (stanya) is formed in the mammary glands (stanyavahi sira) in breasts (stana). Stanyashaya (site of breast milk) is also termed as ‘ksheerashya’ or a part of 'strotas’ comprising of stanyavaha sira present exclusively in females. [Su. Sa. Shareera Sthana 5/10] Blood vessels in chest (vakshagata sira) representing the rakta dhatu are also present in the stana comprising of stanamoola sira, which are two in number. [Su. Sa. Shareera Sthana 5/37, Su. Sa. Shareera Sthana 7/22] It is the abode of two mansa- marma namely ‘Stana-Rohita’ and ‘Stana-Moola’ injury to which can lead to number of complications. [Su. Sa. Shareera Sthana 6/35]
Structural part of stana mainly comprises of mansa dhatu and consists of about 10 peshi (muscles), which are absent in males and undergo physiological hypertrophy during youth. [Su. Sa. Shareera Sthana 5/39] Two dhamani are present in stana of female according to Sushruta. [Su. Sa. Shareera Sthana 9/5] Charak has described normal anatomical positioning, shape and size of stana. [Cha. Sa. Shareera Sthana 8/14] Normal characteristics of stana sampat are not too highly positioned (na-atiurdhwa), not too elongated (na-ati lamba), not much emaciated (anati krisha), not overly nourished (anati peenau), nipples of appropriate size (yukta pippalikau) and nipples not retracted and easy for suckling (sukha prapannau). The description of stana is identical to that given by the modern science. Nipples situated at upper side of breasts (urdhwastana) can lead to visual abnormalities in child. While nipples at elongated side of breasts (lambastana) leads to covering of face of child, which might lead to suffocation. [Su. Sa. Shareera Sthana 10/25, Cha. Sa. Shareera Sthana 8/33] Thus the prenatal and antenatal examination of breast is important to avoid such complications.
Characteristics and diagnostic aspects concerning Stanya
The stanya dushti and its presentation in different neonates can be understood by the application of objective parameters like laboratory investigations and physico-chemical analysis along with the qualitative assessment. Sushruta has thus advised to examine the stanya by putting the drops of stanya in clear water. The appearance of shankha (conch) like white colour and homogeneity of mixture, absence of effervescence (phena), thread like appearance (tantumatva), does not float on the surface (no-utplavati), does not get precipitated) (na avasidati) is considered to be the features of shuddha stanya and keeps the child healthy (aarogya), gives proper growth and development (shareeropachaya) and improves strength (bala vriddhi) in child (kumara). [Su. Sa. Shareera Sthana 10/31]
The different diagnostic parameters concerning the metabolism of stanya are explained in the figure underneath (Figure no. 1)
Pharmacological properties of breast milk
- Rasa (taste): madhura (sweet) and slight astringent (kashaya)
- Veerya (potency): sheeta (cold)
- Guna (quality): light to digest (laghu)
- Useful in nasya (nasal therapy), aschyotana (eye drops), as wholesome (pathya) and vitalizer (jeevana) [Su. Sa. Sutra Sthana 45/57]
- It shall not be boiled [Su. Sa. Sutra Sthana 45/62]
- Curd made out of breast milk possesses unctuous (snigdha), heavy to digest (guru), sweet(madhura) properties. It has balya (strengthening), santarpana (satiating), chakshushya (beneficial for eyes) and doshaghna properties. [Su. Sa. Sutra Sthana 45/73]
- Ghrita (ghee) prepared out of stanya is easy to digest, chakshushya (beneficial for eyes) and anti-toxic (vishaghna) leading to enhancement of agni and nourishing to body.
It is used in the ocular therapies (prasadana putapaaka) for purpose of rejuvenation to eyes. [A.H. Sutra Sthana 24/16] It is also used as a medium for the proper attachment of jalauka(leech) during raktamokshana. [A.H. Sutra Sthana 26/41]
The vitiation of stanya leads to dosha vitiation in the child causing range of diseases. Dalhana mentions that the diseases occur due to consumption of vitiated stanya by the child. [Dalhana on Su. Sutra Sthana 1/7/5] The stana roga like stana-vidradhi (abscess), stana-granthi (cyst) predominantly occur after the development of stana or mammary glands according to the Sushrut Samhita. [Su. Sa. Sutra Sthana 10/17, 26, A.H. Chikitsa Sthana 13/28].
1) Dosha vaishamya (disequilibrium of dosha)
As mentioned earlier the pathology or the vitiation of normal physiology of stanya is the main reason behind the occurrence of diseases in the new-born. The basic dosha disequilibrium (vaishamya) can be understood as depletion (kshaya) and increase (vriddhi). It can be summarized in the table given below:
| Types of Vaishamya | Features | Practical understanding |
|---|---|---|
| Stanya kshaya (depletion state)
(Su. Sa. Sutra Sthana 15/12) |
|
|
| Stanya vriddhi (increased state)
(Su. Sa. Sutra Sthana 15/6) |
|
These conditions are often faced by the practitioners and primi mothers during day to day practice. The stanya kshaya or stanya nasha (reduction in amount of stanya- breast milk) is an important condition as it directly affects the growth and development of new born. Acharya Sushruta has provided the detailed explanation regarding the etio-pathology, clinical features and management of this condition.
- Causes of stanya nasha or stanya kshaya (absence of breast milk or low milk supply):
Krodha (anger), shoka (depression/sorrow), avatsalya (resentment) are mentioned as the most important causes of decreased stanya production as per Sushruta. Vagbhata mentions langhana (fasting) and ayasa (over exertion) in addition to above causes. [Su. Sa. Shareera Sthana 10/30, A.H. Uttar Tantra 1/17] - Treatment of stanya kshaya:
It includes the application of basic concepts pertaining to stanyajanana (facilitating the production of Stanya) and stanyashodhana (alleviation of dosha vitiation in stanya). The treatment can be summarized as given below: [Su. Sa. Shareer Sthana 10/30, Cha. Sa. Shareera Sthana 8/57, A.H. Uttara Tantra 1/18] - Saumanasya janana: Creating and maintaining healthy blissful state of mind
- Diet (aharaja) protocol: One suffering from depletion (stanya kshaya) should consume the dietary items like, yava (barley), godhuma (wheat), shali (rice), mansa rasa (meat soup), sura (wine). Alcoholic preparations like seedhu [Su. Sa. Sutra Sthana 45/175-176, Cha. Sa. Sutra Sthana 27/179, A.H. Sutra Sthana 5/67], sauveeraka (alcoholic preparation), peenyaka (sesame extract), lashuna (garlic, allium sativum), matsya (fish), ksheera prayoga (milk and dairy products), drava-amla- lavana pradhana ahaara (liquid diet predominantly salty and sour in taste), nishpava (flat beans) (A.H. Sutra Sthana 6/20). Sushruta also mentions masha (black gram), rajamasha (cow peas). (Su. Sa. Sutra Sthana 46/34-35)
- Medication/aushadha protocol: Use of herbs like kasheruka (Actinoscirpus grossus (L.f.) Goetgh.), shrungataka (Trapa bispinosa Roxb.), bisa (Nelumbo nucifera Gaertn), vidarikanda (Pueraria tuberosa), madhuka (Madhuca longifolia), shatavari (Asparagus racemosus), nalika (Pergularia daemia (Forssk.)), alabu (Chenopodium album), kaalashaaka (Corchorus capsularis). veerana (Vetiveria Zizanioides), ikshu (Saccharum officinarum), darbha (Desmostachya bipinnata Stapf.), kasha (Saccharum spontaneum) , gundra (Typha angustata) , moolaka (Raphanus sativus L.). [Cha. Sa. Shareera Sthana 8/56]
As mentioned earlier, extensive knowledge and research is available on the lactogenic, galactagogic potential of herbs mentioned in Ayurveda. The dravya like shatavari (Asparagus racemosus), ashwagandha (Withania somnifera), vidari (Pueraria tuberosa), musali (Chlorophytum borivilianum), durva (Cynodon dactylon), haridra (Curcuma longa Linn), musta (Cyperus rotundus), padmaka (Prunus Cerasoides D), guduchi (Tinospora cordifolia). Similarly, other drugs constituting jeevaniya (A.H. Sutra Sthana 15/5), vidarigandhadi (A.H. Sutra Sthana 15/7), padmakadi gana (A.H. Sutra Sthana 15/41), mustadi gana (A. H. Sutra Sthana 15/42, Su. Sa. Sutra Sthana 54-55), vacha-haridradi gana (A. H. Sutra Sthana 15/35-36), vacha-haridradi (Su. Sa. Sutra Sthana 38/26-28), kakolyadi gana (Su. Sa. Sutra Sthana 38/35-36) have proven potent effect in enhancing the breast milk production.[9][10][11][12][13]
Dalhana has also mentioned few treatment modalities like sura (fermented or alcoholic preparations), shali (rice), mansa (meat), goksheer (milk), sharkara (sugar), dadhi (curd), hridya diet in the treatment of stanya kshaya [Dalhana on Su. Sa. Sutra Sthana 15/29-31]
The aparistruta stanya (improper or inadequate expression of breast milk, improper technique of breast feeding), the child can suffer from conditions like kasa (cough), shwasa (breathing difficulties), vami (vomitus) hence breast feeding should be avoided in such conditions. [Su. Sa. Shareera Sthana 10/29]
2) Treatment of stanya dushti as per Sushruta
The rasa dominant in tikta, kashaya, katu and madhura rasa are indicated for this purpose. [Cha. Sa. Shareera Sthana 8/56]
- Panchakarma: Therapeutic emesis (vamana) [A.H. Sutra Sthana 18/2], therapeutic purgation (virechana), therapeutic enema with decoction (asthapana) and unctuous enema (anuvasana).
- Aahara : Yava (barley), godhuma (wheat), shali (rice), mudga (green gram), harenu, kulattha (horse gram), sauveeraka (type of fermented preparation), maireya (type of fermented preparation) , medaka (type of fermented preparation) , lashuna (garlic) , karanja shaka (Pongamia pinnata)
- Herbs: Patha (Cissampelos pareira), mahaushadha (shunthi), suradaru (Cedrus deodara (Roxb)), musta, murva (Marsdenia tenacissima), guduchi, vatsaka (Holarrhena antidysentrica Linn. Wall.), kiratatikta (Swertia chirata), katurohini (Picorrhiza kurroa), sariva(Hemidesmus indicus) in kwatha form.
Etiological factors of stanya dushti
There is also explanation of different etiological factors pertaining to the stanya dushti in samhita which are described below [Cha. Sa. Chikitsa Sthana 30/232-236] (Table No. 2 Showing the involvement of dietary (aaharaja), lifestyle (viharaja) and psychological (manas hetu) in vitiation of stanya.
| Aaharaja hetu (dietary factors) | viharaja hetu
(lifestyle related factors) |
manas hetu
(psychological factors) |
|---|---|---|
| Ajeerna bhojana (eating despite the food is undigested) | Jagarana (night awakenness) | Mana santapa (mental disturbance) |
| Asatmya ahara (eating unwholesome food) | Atichinta (over thinking) | Krodha (anger) |
| Vishama ashana (eating in inappropriate amount and time) | Vegavidharana (suppression of urges ) | |
| Viruddha ahara (eating incompatible food) | Vega udeerana (over expression fof urges) | |
| Atibhojana (over-eating) | Diwaswapna (daytime sleeping) | |
| Amla / ksharayukta/ lavanayukta bhojana (eating food i.e. sour, alkaline and spicy in nature) | Abhighata (injury or accident) | |
| Guda (Jaggery) , krishara (gruel), dadhi (curd) , mandaka (preparation of curd), gramya- udaka- anupa mansa (meat of different animals) |
Ashtang Hridaya has also mentioned viruddha ahara (incompatible diet), kshudha (excessive hunger) , vichetasa (abnormal lifestyle), dhatu dushti as cause of stanya dushti. (A.H. Uttar Tantra 1/19)
Thus all the diet related, lifestyle related and psychological factors are involved in the pathogenesis of stanya dushti (vitiation of breast milk). These can be considered as risk factors for various disorders related to breast milk and breast feeding.
Understanding the clinical features of stanya dushti
Dalhana has pondered over the vitiation of stanya due to various dosha where the stanya vitiated by pitta dosha can lead to pungent and bitter taste instead of sweet. It also leads to occurrence of pita (yellowish discolouration), neela (bluish discolouration), lohita raji (reddish discolouration) in stanya. (Dalhana on Su. Sa. Nidana Sthana 10/25) Atipandutva (excess whitishness) and ati-madhurya (excess sweet taste) is depictive of kapha dushta stanya as well. [Dalhana on Su. Sa. Nidana Sthana 10/25]
Charak Samhita [Cha. Sa. Shareera Sthana 8/56] and Ashtang Hridaya (A.H. Uttar Tantra 2/2-5) also mentions the features of stanya dushti based on dosha prominence as below-
| Stanya dushti | Colour of stanya | Taste (rasa) of stanya | Nature of stanya | Effect of stanya |
|---|---|---|---|---|
| Vataja | Shyava-aruna varna (Reddish black in colour) | Kashaya Anurasa (slightly astringent) |
|
|
| Pittaja |
|
Tikta (bitter), amla (sour), katu (pungent) taste (rasa) |
|
|
| Kapha | Ati-Shukla (excessively white) | Ati-madhura (sweet),
lavana (salty) anurasa |
|
|
Sushruta has stated that breast feeding is contraindicated in mother who is kshudhita (hungry), shokarta (depressed), shranta (exhausted), pradushta dhatu (having dosha and dhatu vitiation), garbhini (pregnant), atiksheena (excessively weak), atisthula (obese), vidagdha bhakta (one consuming spicy food), viruddha ahara (consuming incompatible diet). [Su. Sa. Shareera Sthana 10/31]
Charak explains 8 types of abnormalities in breast milk (ksheera dosha) based on the dosha prominence. [Cha. Sa. Sutra Sthana 19/4/1] The dosha accumulate in mammary glands and ducts (ksheeravaha sira) leading to abnormalities in breast milk. [Cha. Sa. Chikits Sthana 30/236]
The clinical features along with the treatment protocol of these stanya dosha can be summarized as below: [Cha. Sa. Chikitsa Sthana 30/232-235] Treatment of stanya dushti according to Ashtang Hridaya (A.H. Uttar Tantra 2/9-14) is also explained (Table No. 4 treatment of breast milk abnormalities as per Charaka Samhita and Ashtang Hridaya)-
| Type of stanya dushti | Clinical features | Treatment as per Charak Samhita | Chikitsa of Stanya Dushti as per Ashtang Hridaya |
|---|---|---|---|
| Vataja Stanya Dushti | |||
| Vairasya |
|
|
|
| Phena-Sanghata | Kricchra Pravartana (difficulty in expression of breast milk) , Kshamaswarata (dull voice) , Purisha-Mutra Graha (retention of faeces and urine) ,causes Vataja Shiroroga (headache), peenasa (sinusitis) |
| |
| Raukshya | Balahrasa (Weakness) |
| |
| Pittaja Stanya Dushti | |||
| Vaivarnya | Discolouration of Stanya , Gatravaivarnaya (discolouration of body parts) , Swedana-Adhikya (excessive perspiration) , Trishna-Adhikya (excessive thirst) |
|
|
| Vaigandhya | Occurrence of Pandu and Kamala in the child. |
| |
| Kaphaja Sthanya Dushti | |||
| Sneha | Chardana (vomitus), Kunthana (discomfort or pain), Lalastrava (excessive salivation), Strotas Rodha (obstruction of body channels), Nidra (sleepiness), Klama (lethargy). |
|
|
| Paichillya | Lalastrava , Vaktra-Shotha (Inflammation in the buccal cavity) |
| |
| Gaurava | Hridroga (Heart disorders) |
|
|
| Tridoshaja Stanya Dushti | |||
| Tridoshaja |
|
| |
It can be observed that the treatment protocol of each abnormality involves use of internal medicine with the external application of different drugs over the breast region of lactating mothers.
Diseases in neonates due to abnormal breast milk
- Sushruta mentions the consumption of heavy to digest food, inappropriate quantity and untimely food intake leads to abnormal breast milk. This causes diseases in neonate. [Su. Sa. Shareera Sthana 10/33]
- Ashtang Sangraha explains the variety of diseases like jwara (fever), kasa (cough), chhardi (nausea, vomiting, gastric disturbance) commonly observed in the paediatric population. (A. S. Uttar Tantra 1/22)
- Ksheeralasaka and Parigarbhika are two most common diseases observed in neonates. These conditions are explained by focusing on the growth and development of new-born. Ksheeralasaka (A.S. Uttar Tantra 2/20-22) is a condition involving the vitiation of all the three dosha resulting in symptoms like diarrhoea, malaise, fever, vomiting, nausea etc. in the child. This is comparable to the chronic indigestion and disturbed gastro-intestinal functioning, which is commonly observed in breast fed infants.
- Parigarbhika is popularly understood as the failure to thrive or malnutrition related disorders. It has been explained as an important factor resulting from the abnormal breast milk. [A.S. Uttar Tantra 1/23]
- Deepana treatment mentioned in this condition has significant practical application. Similarly, other conditions like kukunaka (opthalmia neonatarum) and ahiputana (napkin rash), [Su. Sa. Chikitsa Sthana 20/57] charmadala (skin disorders) (K. S. Khila Sthana 15/10), utfullika (H. S .3.54.9-13), visarpa (herpetic rash) (K.S Khila Sthana 14/10-15) also result from vitiated stanya leading to the occurrence of range of disorders in the paediatric population.
- Aversion of the infant towards breast feeding (stanya dwesha) is considered a sign of graha dushti e.g. skanda, skandapasmara, andhaputana. [Su. Sa. Shareera Sthana 10/51, A.H. Uttar Tantra 3/5]. It is also observed in conditions like mukha roga (pathologies in buccal cavity), kantha roga (pathologies in throat), trishna (morbid thirst), udarashool (pain in abdomen). The abnormalities in breast milk should be managed by administrating the snehapana in the form of ghrita followed by vamana with water processed with neem (nimba-udaka). [Su. Sa. Chikitsa Sthana 17/42] Stanya pravritti (expression of breast milk) can also be pathologically observed in conditions like rakta gulma without the evidence of pregnancy. [Cha. Sa. Nidana Sthana 3/13, A.H. Sutra Sthana 11/51]
Herbs used in treatment of abnormalities of breast milk
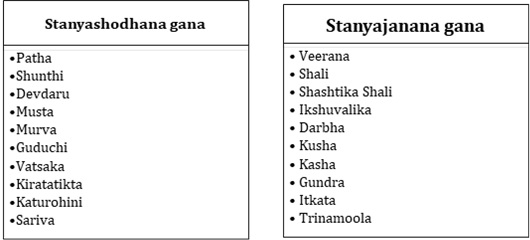
Charaka Samhita dedicates two groups to summarize the treatment protocol of stanya related disorders. These include stanyashodhana (purifiers) and stanyajanana (galactogogues) gana. [Cha.Sa. Sutra Sthana 4/12] The former involves the study of drugs that help to pacify the stanya-dushti and later represents the drugs that help to increase the production and quantity of stanya. (Figure No. 2- Stanya shodhana and Stanyajanana Gana)
It can be observed that the dravya representing the stanyashodhana gana are of katu-tikta rasa pradhanya (dominance of pungent and bitter taste) and ushna veerya (having hot potency) while those in the stanyajanana gana (promoting breast milk production) possess madhura rasa and vipaka. The tikta rasa is explained to have stanya-shodhana (A. H. Sutra Sthana 10/14) and while the madhura rasa possesses stanyakrita (enhancing production of stanya) or stanya-prasadana (enhancing quality of stanya) properties. (A.H. Sutra Sthana 10/8) The excessive consumption of katu rasa on the other hand leads to Ssanya nasha or diminution in production of stanya (Cha. Sa. Sutra Sthana 26/43/5, Su. Sa. Sutra Sthana 42/9/1,4)
Stanya also acts as a medium for the administration of medication i.e. Anupana for the child in ksheerapa state (exclusively breast feeding) and ksheerannada stage (intermittent breast feeding) (Su. Sa. Shareera Sthana 10/37). Ashtang Hridaya suggests the navaneet (butter) with stanya as anupana for 2 kaala (two times per day) during the first few days after birth of new-born (A.H. Uttar Tantra 1/14)
Stanyajanana gana is also indicated as a part of rasayana kalpa (rejuvenating herbs). Hence proper rasayana can be advised for the purpose of stanya vriddhi (increased production of breast milk) (Cha. Sa. Chikitsa Sthana 1/3/3)
There is explanation of dosha dependant treatment protocol with respect to the stanya especially the stanya dushti(vitiation of breast milk) in Charak Samhita. Charak has indicated ksheeravanti madhura dravya (sweet substances processed in milk)(Cha. Sa. Chikitsa Sthana 30/298) as a form of medicine in the children. There is indication of providing the treatment to mother in order to correct the breast milk vitiation. Thus the indicated medication can be delivered by mixing it with the mother’s milk to achieve better results.
Stanyapana vignyana (breast feeding techniques) and substitutes to breast feeding
The substitutes for breast milk are described as below: [Su. Sa. Shareera Sthana 10/47, A.H. Uttar Tantra 1/20]
- Chhaga paya (goats milk): It is considered to be best when breast milk is not available. [Cha. Sa. Sutra Sthana 25/42]
- Gavya paya (cow milk) : It is also mentioned to be one of the best substitute for breast milk [A.H. Sutra Sthana 5/22] Contemporary science states that raw and unpasteurised cows milk is difficult to digest and contain more protein content like casein as compared to human milk. The infant formula milk is however treated bovine milk making it a appropriate substitute for breast milk.[14] The goats milk based infant formula can also be administered as a substitute in case of cow milk allergy but can result in nutrient deficiency.[15]
- Laghu- panchamula siddha ksheera with sitopala or sthiradi varga siddha kshira with sitopala - Laghu Panchamula consists of roots of 5 herbs namely , Shalaparni (Desmodium gangeticum), Prishniparni (Uraria picta) , Brihati (Solanum indicum), Kantakari (Solanum virginianum) and Gokshura (Tribulus Terrestris). Research proves that these herbs have proven galactogogue activity[16] These can be used as substitutes for formula milk or breast feeding in the circumstances where breast feeding is not possible. The evidence based scientific preclinical study and clinical trials should be carried out to prove the effectiveness of the mentioned options.
Contra-indications to breast feeding
Breast feeding is contraindicated in the conditions like atikshudha (excessive hunger), shoka (depression), shranta (tiredness), in the illnesses like jwara, kshaya, sthoulya, in individuals consuming the vidagdha and viruddha ahara. [Su. Sa. Shareera Sthana 10/30] It is also not indicated in the child who is suffering from ajeerna . Here the digestive power (agni) also plays a vital role in determining the outcomes. Thus a study can be carried out to assess the effect of enlisted factors on the stanya and the child. These could be achieved through robust cohort, case control or cross-sectional observational studies.
Concept of dhatri or wet nurse
Breast feeding is started as soon as lactation starts or at least within the 3 to 4 days of post-natal period. [Su. Sa. Shareera Sthana 10/14] Dhatri or wet nurse feeds the infant in case of the inability of breast feeding by the mother. The dhatri should be in the state of optimum health and conduct in order to provide best nutrition to the baby. This can be understood as the application of concept of formula feed or breast milk storage or obtaining the same from the milk banks to ensure the nutrition of child. According to Sushruta, the dhatri must be of sama varna (of same ethnicity), madhyama pramana (medium built), madhya vaya (middle aged), aroga (disease free), sheelavati (with good character), achapala (not impatient), alolupa (satisfied), akrisha (not too thin), asthula (not too fat), avyanga (not having any disability), avyasani (devoid of any addictions), prasanna ksheera (breast milk is not vitiated), vatsala (caring and loving), jeevatvatsa (whose infant is alive). [Su. Sa. Shareera Sthana 10/25, Cha. Sa. Shareera Sthana 8/52] Ashtang Hridaya advises two dhatri or nursing mothers. [A. H. Uttar Tantra 1/15-16] Sushruta mentions to commence the breast feeding from right breast first after proper mantroccharana (chanting of mantra). [Su. Sa. Shareera Sthana 10/25-27]
Weaning is explained to be done between 6 months to 1 year of age mostly after the appearance of teeth in the infant. Annaprashana vidhi (introduction to food) is indicated at this stage for the introduction of complementary feeds. [Su. Sa. Shareera Sthana 10/35] Various dietary options in the form of modaka, lehana (lickables) are mentioned for the purpose of annaprashana. Here the sequential increase in food quantity (kramatyaga vidhi) and weaning should be followed. Ayurveda modalities can be followed to promote the process of complementary feeds and supplementary nutrition during the weaning period.
Research on use of stanya as a therapeutic agent in disorders of adult population
Ayurveda has also explored the pharmacological activity?? of stanya in systemic conditions related to the adult population. Stanya has activities lik jeevana (vitalizer), brihana (nourishing), satmya (wholesome), snehana (unctuous) and leads to alleviation of vata- pitta dosha. [Cha. Sa. Sutra Sthana 27/224, A.H. Sutra Sthana 5/26] There is description regarding the use of stanya for the purpose of nasya (nasal instillation), tarpana, seka or aschyotana (eye drop instillation) in the diseases of eye. [Cha. Sa. Sutra Sthana 27/223] It is indicated in the management of raktapitta vyadhi, [Cha. Sa. Sutra Sthana 27/222] hikka [Cha. Sa. Chikitsa Sthana 17/131] for the purpose of nasal instillation and oral consumption; pittaja abhishyanda for purpose of anjana [Su. Sa. Uttar Tantra 10/9], in conditions like abhighata (injury to the organs). (A.H. Sutra Sthana 5/26)
Recent advances on the research data available on concept of stanya
Researches on experimental studies exploring the galactagogic activities of various ayurveda herbs are observed. Few clinical trials measuring the galactogogue activity were also obtained. Findings of some of these articles can be summarized as below –
Studies focusing on the physiological and pathological aspects considering the stanya
- In the article , “Noxious Alterations in Human Milk: An Ayurveda Perspective[17]” is related with the understanding of causes of vitiation of human milk, its effect on composition of human and to critically analyse the effect of consumption of vitiated milk on the infant.
- Breast milk as an etiological factor in infantile disorders – An observational study[18] The breastmilk from 100 mothers with infants in age group of 1-6 months was collected and subjected to organoleptic and laboratory tests to identify the type of stanya sushti.
- In the article, ‘Understanding the Concept of Stanya and its Need in Context to Breastfeeding’[19], the authors have underlined the importance of breast feeding in context to concept of Stanya in Ayurveda.
- The article, The Concept Of Stanya Apanayana (Weaning)[20] focuses on the concept of Stanya apanayana i.e. weaning according to the classical texts in detail.
- The observational study entitled, Biochemical Analysis Of Stanya & Its Correlation With Rasa-Sarata[21], the lipid profile along with the Rasa Saarata of lactating mothers was assessed in the present study showing strong positive correlation between the Stanya and Rasa Saarata.
- The article An ayurvedic perspective of hypoprolactenemia: Stanyakshaya[22] explores the concept of Stanya Kshaya in Ayurveda in perspective of hypoprolactenemia.
- The study, Stanyajanan drugs in Bhavprakasha Nighantu - a review Article[23] the understanding of stanya physiology in light of contemporary medical science is explained in detail in the article.
- The author has compared the condition of ksheeralasaka with cow milk allergy and implications it can pose upon the health and wellbeing of child in the article entitled, Ksheeralasaka Vis-À-Vis Cow’s Milk Allergy: A Critical Review[24]
- The article, A scientific understanding of mammary gland and physiology of lactation in Ayurveda[25] the physiology of lactation is widely explained.
- In the article , Explication on tissue nutrition in prenatal and postnatal life: An Ayurveda perspective[26] the authors have beautifully elaborated the nutrition related metabolism mentioned during the intrauterine and postnatal life of infant.
- In the article, Concept of Dhatri (wet nurse) in perspective of Ayurveda w.r.t. Babylonian Code of Hammurabi[27] the historical aspects regarding the tradition of wet nurse and ethical considerations are discussed. The study states that the concepts of wet nurse is as old as the proofs Babylon code.
- In the article, Breastfeeding assessment protocol: An integrated approach[28] the authors have extensively described the breast feeding protocol and assessment to ensure the health of newborn and lactating mothers. This can also be used as reference for further studies.
- In the study, An Ayurvedic Review on Phakka Roga w.s.r. To Rickets in children[29] the detail analysis of Phakka Roga as a consequence of Stanya Dushti leading to nutritional deficiency like rickets is done in the present article.
Herbal drugs for nourishment of stanya
- Many herbal galactogogues have like Shatavari (Wild Asparagus) and Ashwagandha (Withanina) are extensively studied in contemporary sciences as well. Various systematic reviews are done to generate bulk data regarding the same.[30][31]
- Similarly extensive studies have been done on the evaluation of the galactogue potential of single herb like Musta (Cyperus rotundus)etc. Preclinical study entitled as “The Evaluation of a lactogenic activity of an aqueous extract of Cyperus rotundus Linn”[32] revealed that the the aqueous extract of Cyperus rotundus can stimulate milk production in the female rats.
- The article, The Potential of Medicinal Plants as Galactagogue in Indonesia: A Review from Medical Perspective the ethnobotanical review galactagogue effect and breast milk promoting effect of different herbs native to Indonesia is elaborated.[33]
- The study “ Botanical galactogogues: nutritional values and therapeutic potentials” focuses on the nutritional and therapeutic effect of selective herbal plants from the family like Verbenaceae, Bignoniaceae, Sapindaceae, Amaranthaceae, Asclepiadaceae, Bombacaceae, Sapindaceae, and Asteraceae.[34]
Clinical Studies considering the aspects of stanya
- The article “Clinical Study on Plant Galactagogue Worldwide in Promoting Women’s Lactation: a Scoping Review[35]”, is a systematic review on the different herbs analysed for their clinical galactagogic activity.
- The article, A Double-Blind Randomized Clinical Trial for Evaluation of Galactogogue Activity of Asparagus racemosus Willd.[36] is a randomized double-blind clinical trial evaluates galactogogue effect of Shatavari in 60 lactating mothers by evaluating their prolactin hormone level during the study.
- The article, Stanyakshya (insufficient lactation) and its management by an Ayurveda formulation: A case report[37] mentions the positive effect Kwath prepared with Shatapushpa, Dhanyaka, Jeeraka, Methi used traditionally in Rajasthan which was administered in women with insufficient lactation. This intervention showed encouraging results.
- In the research study, To Evaluate the efficacy of Aahara –Vihara on Stanya Kshaya in Healthy Female Volunteers of different Deha Prakriti[38] the effect of dietary and lifestyle intervention on Stanya Kshaya is explored. The study included the dietary interventions in women of Stanya Kshaya. Most of the women were of Vata-Kapha Prakriti and dietary interventions showed benefit in their condition.
- The efficacy of different Gana mentioned in the management of Stanya Kshaya is also assessed clinically. For instance, the article, Haridradi Gana Kwatha in the Management of Stanya Kshaya w.s.r To Hypogalactia - A Clinical Study[39] depicted that the Haridradi Gana kwatha has promising results in the management of all the parameters of Stanya Kshaya.
- The study entitled. A Comparative study of Madhuk Churna with Vidarikanda Churna in the management of Stanyakshaya[40] showed encouraging results in management of Stanya Kshaya. The authors have compiled the different Stanyajanana herbs in Bhavaprakash Nighantu
- The article, Role of Stanyashchotan (topical application of Breast milk) in Opthalmia Neonatorum - a case study[41] discusses the pharmacological effect of topical application of Stanya in condition of Opthalmia Neonatarum leading to significant relief in symptoms.
Contemporary approach
Physiology of Lactation-
The initial growth of mammary glands starts with thelarche at puberty while the duct system and glandular tissue develops for the production of milk just before gestation under the influence of hormones estrogen and progesterone. Prolactin is necessary for milk secretion and proliferarion of epithelial cells of mammary alveoli. Thus the physiological aspects related to initiation of milk secretion (lactogenesis) and maintenance of milk secretion (galactopoiesis) is dependant on hormones via hypothalamo-pituitary axis. Milk ejection is dependant on suckling by the infant and is a neuro-endocrine reflex initiated via the oxytocin.[42]
Composition of Breast Milk
Human milk forms the primary source of nutrition for infants. It contains about 88.5% of water and 11.5% of solids. The breast milk secreted before parturition and in initial post natal period is termed as colostrum at rate of 40ml a day. It also contains lactose, lactalabumin, iron, Vitamin A and D and minerals. It also contains several antibodies (Immunoglobulins- IgA), phagocytes, macrophages important for the protection of infants from microbial attack.[43] The colostrum contains low fat content but more protein. During the 2nd and 3rd weeks after birth there is change in composition of breast milk where it becomes rich in fats and sugars and its calorific value also increases. This is termed as transitional milk. By the time baby is 3 weeks old, the milk attains mature composition making it high in fats, sugars, essential amino acids, is iso-osmotic with plasma with high calorific value.[44] The composition of human breast milk can be expressed in table as given below (Table No. 4)-
| Breast milk content | Colostrum | Transitional milk | Mature Milk | ||
|---|---|---|---|---|---|
| Total Fats (g/L) | 30 | 35 | 45 | ||
| Total Protein (g/L) | 23 | 16 | 11 | ||
| Lactose (g/L) | 57 | 64 | 71 | ||
| Total Solids (g/L) | 128 | 133 | 130 | ||
| Calorific value (MJ/L) | 2.81 | 3.08 | 3.13 | ||
Contradictions to breast milk feeding[45]-
- Temporary – Fissuring or crackling of nipples, mastitis, acute illness of mother
- Permanent- Galactosaemia, poor nutrition, debility, postpartum psychosis, breast abscess, HIV or Hepatitis B infected mothers (chance of infection transmission upto 25%)
Treatment of low breast milk output
In case of low breast milk output , the drugs like Chlorpromazine or Metoclopramide are prescribed along with dietary and psychological advice for the mother. In case of sick or preterm infants the breast milk is expressed manualy or pump and fed by cup, spoon or tube. It can be preserved at room temperature for 6 hours and in refrigerator for 24 hours at 4-8 degree Celsius without contamination.
The artificial feeding can involve use of whole fresh milk (buffalo, cow), skimmed milk, toned milk, powdered milk (whole milk powder/skim milk powder/humanised milk powder), modified milk powder (animal fat is substituted with vegetable fats, fortified with iron and vitamins), soyabean milk.
| Milk (per 100ml) | Human | Cow | Buffalo | Double toned | Toned
(Buffalo) |
|---|---|---|---|---|---|
| Protein | 1.2 | 3.5 | 4 | 3 | 3 |
| Fat | 4 | 4 | 7 | 1.5 | 3.5 |
| Carbohydrate
(Lactose) |
7 | 4 | 4 | 4 | 4 |
| Calories | 67 | 67 | 103 | 40 | 67 |
Milk banks have now emerged as important source for the storage and dispensing of the donor breast milk to the infants who may stay devoid of mothers milk due to variable reasons. These are being established across the globe to meet the long term demand.[46] Extensive research is being carried out to promote the breast feeding and establishment of milk banks also supported by the organisations like UNICEF and WHO.[47]
Weaning
The breast milk is sole and sufficient source of nutrients from birth to about 6 months. Complimentary feeds are offered after 4-6 months of age. The solid food is introduced gradually to the infant after this period. Green banana , mashed vegetable, dal is initially introduced while eggs and meat is given after 9 months.
Related Adhyaya
- Yonivyapat Chikitsa Adhyaya [Cha. Sa. Chikitsa Sthana 30]
- Grahani Dosha Chikitsa Adhyaya [Cha. Sa. Chikitsa Sthana 15]
- Shareera Sankhya Shareera Adhyaya [Cha. Sa, Shareera Sthana 7]
- Jaatisutriya Shareera Adhyaya [Cha. Sa, Shareera Sthana 8]
- Doshadhatumalavriddhikshaya Vignyaniya Adhyaya [Su. Sa. Sutra Sthana 15]
- Balopacharniya Adhyaya [A.H. Uttar Tantra 1]
- Balamaya Pratishedha Adhyaya [A.H. Uttar Tantra 2]
- Balagraha Pratishedha Adhyaya, [A.H. Uttar Tantra 3]
- Lehanadhyaya [Kashyap Samhita]
- Ksheerotpatti Adhyaya [Kashyap Samhita]
- Ksheerguna Vishesha Adhyaya [Kashyap Samhita]
Send us your suggestions and feedback on this page.
References
- ↑ MONIER-WILLIAMS, M. (1872). A Sanskṛit-English dictionary, Page No. 1142
- ↑ Gadgil N, Kulkarni A. An observational study to quantify the measure of Anjali Pramana -A pilot study. 1 Neha Dattatraya Gadgil, and. 2019 Jul 27;
- ↑ Kent, J. C., Gardner, H., & Geddes, D. T. (2016). Breastmilk Production in the First 4 Weeks after Birth of Term Infants. Nutrients, 8(12), 756. https://doi.org/10.3390/nu8120756
- ↑ Shah R, Sabir S, Alhawaj AF. Physiology, Breast Milk. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [cited 2023 May 12]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK539790/
- ↑ Riddle SW, Nommsen-Rivers LA. Low milk supply and the pediatrician. Curr Opin Pediatr. 2017;29(2):249-256. doi:10.1097/MOP.0000000000000468
- ↑ Haney AF. Galactorrhea. Curr Ther Endocrinol Metab. 1997;6:393-396.
- ↑ Reisenbichler E, Hanley KZ. Developmental disorders and malformations of the breast. Semin Diagn Pathol. 2019;36(1):11-15. doi:10.1053/j.semdp.2018.11.007
- ↑ Ajao OG, Ajao AO. Breast abscess. J Natl Med Assoc. 1979;71(12):1197-1198.
- ↑ Patil DPD, Bhalgat DMS. WJPR - Abstract. 1 [Internet]. [cited 2023 Jul 10]; Available from: https://wjpr.net/abstract_show/12611
- ↑ Gulshan. Padmakadi Gana - Group of Ayurvedic Herbs [Internet]. 2017 [cited 2023 Jul 10]. Available from: https://www.ayurmedinfo.com/2012/04/23/padmakadi-gana-group-of-ayurvedic-herbs/
- ↑ Apila Nath M.K, N.Sudhakar, Sarojini Byadagi, Binu.M.B. Haridradi Gana Kwatha in The Management of Stanya Kshaya w.s.r to Hypogalactia - A Clinical Study. International Journal of Ayurveda and Pharma Research. 2020;8(Suppl 1):19-24.
- ↑ Dipti, et al. Vidarigandhadi Gana of Sushruta Samhita: A Review of its Clinical Indications. Nat Ayurvedic Med 2020, 4(3): 000262. Ayurvedic Medicine. 2020;
- ↑ Kumar B. A REVIEW ON KAKOLYADI GANA OF SUSHRUTA SAMHITA. Indian Journal of Agricultureand Allied Sciences,Vol 4, Issue No.: 2 , page No 80-82
- ↑ Martin, C. R., Ling, P. R., & Blackburn, G. L. (2016). Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients, 8(5), 279. https://doi.org/10.3390/nu8050279
- ↑ British Journal Of Midwifery [Internet]. [cited 2023 Jul 10]. British Journal Of Midwifery - Alternatives to breastfeeding: The use of goats’ milk in infant formula. Available from: https://www.britishjournalofmidwifery.com/content/clinical-practice/alternatives-to-breastfeeding-the-use-of-goats-milk-in-infant-formula/
- ↑ Ghildiyal, S., & Joshi, V. K. (2012). A critical review on two types of Laghupanchamula. Ayu, 33(3), 343–347. https://doi.org/10.4103/0974-8520.108820
- ↑ Londhe D, Chinchalkar S, Chiluveri AC, Kumar S, Chiluveri SK. Noxious Alterations in Human Milk: An Ayurveda Perspective. J Hum Lact. 2022;38(2):332-338. doi:10.1177/08903344211032130
- ↑ Meti R, Ankad G. Breast milk as an etiological factor in infantile disorders - An observational study. J Ayurveda Integr Med. 2021;12(4):700-704. doi:10.1016/j.jaim.2021.06.011
- ↑ Tanwar K, Tanwar A.K “Understanding The Concept of Stanya And Its Need In Context To Breastfeeding IRJAY.[online]2022;5(2);179-183.Available from: https://irjay.comDOI: https://doi.org/10.47223/IRJAY.2022.523
- ↑ Konapalli J, Krishnaiah N. The Concept Of Stanya Apanayana (Weaning). Int J Ayu Pharm Res [Internet]. 2018Dec.9 [cited 2023May12];6(10). Available from: http://ijaprs.com/index.php/ijapr/article/view/1075
- ↑ Rai S, Versha P, Sawhney S. Biochemical Analysis Of Stanya & Its Correlation With Rasa-Sarata, WJPR, Volume 10, Issue 7, Page No. 814-823
- ↑ Meher S, Jayasingh BK. AN AYURVEDIC PERSPECTIVE OF HYPOPROLACTENEMIA: STANYAKSHAYA, WJPR, Volume 11, Issue 9, Page No. 492-500.
- ↑ Uike CS, Landge ST. Stanyajanan drugs in Bhavprakasha Nighantu-A Review., WJPR, VOLUME 8, ISSUE 10, 408-412
- ↑ Antony C. Ksheeralasaka Vis-À-Vis Cow’s Milk Allergy: A Critical Review. Int J Ayu Pharm Res [Internet]. 2018Jul.28 [cited 2023May12];6(6). Available from: http://www.ijaprs.com/index.php/ijapr/article/view/984
- ↑ Verma V, Agrawal S, Gehlot S. A scientific understanding of Mammary gland and physiology of lactation in Ayurveda. 2020 Jun 24;10:1–4.
- ↑ Agrawal S, Verma V, Gehlot S. Explication on tissue nutrition in prenatal and postnatal life: An Ayurveda perspective. Journal of Ayurveda and Integrative Medicine [Internet]. 2021 Jan 1 [cited 2023 May 12];12(1):198–205. Available from: https://www.sciencedirect.com/science/article/pii/S097594761830682X
- ↑ Kiran Tawalare, Sumedh Meshram, Pankaj Jogi, Maneesha Kothekar, Pooja Chandak. Concept of Dhatri (wet nurse) in perspective of Ayurveda w.r.t. Babylonian Code of Hammurabi. J Ayurveda Integr Med Sci 2021;1:125-129
- ↑ Thomas P, Jayavarma MK. Breastfeeding assessment protocol: an integrated approach, J Res Educ Indian Med, July - Dec., 2014: XX (3-4):153-163
- ↑ Shelke DSB, Chavan DDB. An Ayurvedic Review On Phakka Roga W.S.R. To Rickets In Children. World Journal of Pharmaceutical Research, Vol 11, Issue 7, 2022 , Page No. 994- 1000
- ↑ Mortel M, Mehta SD. Systematic Review of the Efficacy of Herbal Galactogogues. Journal of Human Lactation. 2013;29(2):154-162. doi:10.1177/0890334413477243
- ↑ Bazzano AN, Hofer R, Thibeau S, Gillispie V, Jacobs M, Theall KP. A Review of Herbal and Pharmaceutical Galactagogues for Breast-Feeding. Ochsner J. 2016;16(4):511-524.
- ↑ Badgujar SB, Bandivdekar AH. Evaluation of a lactogenic activity of an aqueous extract of Cyperus rotundus Linn. J Ethnopharmacol. 2015;163:39-42. doi:10.1016/j.jep.2015.01.019
- ↑ Khairani A. F, Adzdzikri T. M, Menggala S. T, Bashari M. H, Rohmawaty E, Achadiyani A, Kania N. The Potential of Medicinal Plants as Galactagogue in Indonesia: A Review from Medical Perspective. Biomed Pharmacol J 2021;14(3).
- ↑ Gbadamosi I, Okolosi O. Botanical galactogogues: nutritional values and therapeutic potentials. Journal of Applied Biosciences [Internet]. 2013 Feb 19 [cited 2023 Jul 12];61:4460–9. Available from: https://www.ajol.info/index.php/jab/article/view/85594
- ↑ Kwan SH, Abdul-Rahman PS. Clinical Study on Plant Galactagogue Worldwide in Promoting Women's Lactation: a Scoping Review. Plant Foods Hum Nutr. 2021;76(3):257-269. doi:10.1007/s11130-021-00901-y
- ↑ Gupta M, Shaw B. A Double-Blind Randomized Clinical Trial for Evaluation of Galactogogue Activity of Asparagus racemosus Willd. Iran J Pharm Res. 2011;10(1):167-172.
- ↑ Sharma U, Sharma S. Stanyakshya (insufficient lactation) and its management by an Ayurveda formulation: A case report. J Indian Sys Medicine 2022;10:192-5
- ↑ Kiran Tanwar, Uma Shankar Sharma, Ankur Kumar Tanwar. To Evaluate the efficacy of Aahara –Vihara on Stanya Kshaya in Healthy Female Volunteers of different Deha Prakriti. J Ayurveda Integr Med Sci [Internet]. 2016Jun.30 [cited 2023May12];1(01):1-. Available from: https://jaims.in/jaims/article/view/1
- ↑ Apila Nath M.K, N. Sudhakar, Sarojini Byadagi, Binu.M.B. Haridradi Gana Kwatha in The Management of Stanya Kshaya w.s.r to Hypogalactia -A Clinical Study. International Journal of Ayurveda and Pharma Research. 2020;8(Suppl 1):19-24.
- ↑ Dr. Pravin A. Patil, Dr. Anjali N. Lade, & Dr. Chetna J. Kulkarni. (2019). A Comparative study of Madhuk Churna with Vidarikanda Churna in the management of Stanyakshaya. Journal of Ayurveda and Integrated Medical Sciences, 4(02), 11-13. https://doi.org/10.21760/jaims.v4i02.587
- ↑ Kale DY, Choure S. Role of stanyashchotan (topical application of breast milk) in Opthalmia Neonatorum - a case study. World Journal of Pharmaceutical Research, Volume 9, Issue 7, Page No. 2758-2763
- ↑ Sembulingham K , Sembulingham P, Essentials of Medical Physiology,Mammary glands and Lactation, Seventh Edition , Jaypee Health Sciences Publisher, New Delhi , Page No. 530-533
- ↑ Hall J , Hall M , Guyton and Hall Textbook of Medical Physiology, 3rd South Asian Edition , published by Elsevier publishers , Page No. 726-727.
- ↑ Pocock G , Richards C , Richards D , Oxfords Human Physiology , Fifth edition , Oxford University Press, United Kingdom, Page No. 813.
- ↑ 45.0 45.1 Golwalla A, Golwalla S, Golwalla’s Medicine for Students, Twenty Fifth edition , reprinted 2018, Jaypee Brothers Medical Publishers , Page No. 795 to 797.
- ↑ Kim, J., & Unger, S. (2010). Human milk banking. Paediatrics & child health, 15(9), 595–602.
- ↑ Research on supporting breastfeeding - Baby Friendly Initiative [Internet]. [cited 2023 Jul 12]. Available from: https://www.unicef.org.uk/babyfriendly/news-and-research/baby-friendly-research/research-supporting-breastfeeding/supporting-breastfeeding-research/