Difference between revisions of "Congenital disorders"
| (7 intermediate revisions by 3 users not shown) | |||
| Line 2: | Line 2: | ||
|title=Congenital Disorders | |title=Congenital Disorders | ||
|titlemode=append | |titlemode=append | ||
| − | |keywords=congenital disorders, beeja, beejabhaga, beejabhagaavayava, genetics in | + | |keywords=congenital disorders, beeja, beejabhaga, beejabhagaavayava, genetics in Ayurveda, Causes of congenital disorders, preconception care in Ayurveda, prevention of congenital disorders, Ayurveda, Indian system of medicine, Charak Samhita |
| − | |description=Congenital disorders are disabilities or malformations present at or before birth.Ayurveda emphasizes on prevention of congenital disorders through proper preconception, ante- natal and intra partum care. | + | |description=Congenital disorders are disabilities or malformations present at or before birth. Ayurveda emphasizes on prevention of congenital disorders through proper preconception, ante- natal and intra partum care. |
|image=http://www.carakasamhitaonline.com/resources/assets/ogimgs.jpg | |image=http://www.carakasamhitaonline.com/resources/assets/ogimgs.jpg | ||
|image_alt=carak samhita | |image_alt=carak samhita | ||
|type=article | |type=article | ||
}} | }} | ||
| − | '''Understanding | + | '''Understanding congenital disorders in [[Ayurveda]] and contemporary research''' |
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
Congenital disorders are disabilities or malformations present at or before birth. These are identified in prenatal life or at birth, or many years later. As per the World Health Organization, congenital anomalies are a leading cause of neonatal deaths. Every year an estimated 295 000 newborns die within 28 days of birth due to congenital anomalies. These can contribute to long-term disability, with significant impacts on individuals, families, healthcare systems, and societies. <ref>Available from https://www.who.int/news-room/fact-sheets/detail/congenital-anomalies accessed on 15/06/2021</ref> | Congenital disorders are disabilities or malformations present at or before birth. These are identified in prenatal life or at birth, or many years later. As per the World Health Organization, congenital anomalies are a leading cause of neonatal deaths. Every year an estimated 295 000 newborns die within 28 days of birth due to congenital anomalies. These can contribute to long-term disability, with significant impacts on individuals, families, healthcare systems, and societies. <ref>Available from https://www.who.int/news-room/fact-sheets/detail/congenital-anomalies accessed on 15/06/2021</ref> | ||
| − | Human genetics studies individual genes, their role and function in disease, and their mode of inheritance. Genomics refers to an organism's entire genetic | + | Human genetics studies individual genes, their role and function in disease, and their mode of inheritance. Genomics refers to an organism's entire genetic information, the genome,and the function and interaction of DNA within the genome, as well as with environmental or nongenetic factors such as a person's lifestyle. Characterization of the human genome in genomic studies has supported genetics to elucidate the etiology, pathogenesis of the disease, and improve therapeutic interventions and outcomes. The impressive advances in genetics, genomics, and health care information technology have significantly increased the wealth of knowledge. It is helpful in medical practice and play a prominent role in the diagnosis, prevention, and treatment of disease.<ref>J. Larry Ja meson, Peter Kopp. Principles of Human Genetics. In Harrison’s principles of internal medicine. 19th edition. Pg. 425. </ref> |
The ancient rishis of [[Ayurveda]] had recognized the genetic basis of diseases. They have documented the knowledge in various contexts. The current medical system focuses on the identification of genes responsible for diseases. At the same time, the references found in [[Ayurveda]] texts indicate the causes of genetic disorders and their role in health and diseases. A proper study to bridge the gaps and connect these two pools of information can reveal significant insights for a comprehensive understanding of why and what of congenital and genetic disorders. The present article describes congenital disorders in [[Ayurveda]] texts and contemporary research. | The ancient rishis of [[Ayurveda]] had recognized the genetic basis of diseases. They have documented the knowledge in various contexts. The current medical system focuses on the identification of genes responsible for diseases. At the same time, the references found in [[Ayurveda]] texts indicate the causes of genetic disorders and their role in health and diseases. A proper study to bridge the gaps and connect these two pools of information can reveal significant insights for a comprehensive understanding of why and what of congenital and genetic disorders. The present article describes congenital disorders in [[Ayurveda]] texts and contemporary research. | ||
</div> | </div> | ||
| Line 44: | Line 44: | ||
==Congenital disorders as per [[Ayurveda]]== | ==Congenital disorders as per [[Ayurveda]]== | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
| − | In [[Ayurveda]], the congenital disorders are considered incurable(asadhya) with poor prognosis. Similarly, some hereditary of familial (kulaja) ailments are also explained as incurable. E.g. | + | In [[Ayurveda]], the congenital disorders are considered incurable(asadhya) with poor prognosis. Similarly, some hereditary of familial (kulaja) ailments are also explained as incurable. |
| + | |||
| + | E.g. Congenital or hereditary obstinate urinary diseases including diabetes (Jataja prameha) [Cha. Sa. [[Chikitsa Sthana]] 6/57] | ||
Ayurveda emphasizes on prevention of congenital disorders through proper preconception, ante- natal and intra partum care. The causes for congenital disorders are explained in detail. These are helpful in taking necessary actions to avoid such risk factors and obtaining a healthy progeny. | Ayurveda emphasizes on prevention of congenital disorders through proper preconception, ante- natal and intra partum care. The causes for congenital disorders are explained in detail. These are helpful in taking necessary actions to avoid such risk factors and obtaining a healthy progeny. | ||
</div> | </div> | ||
| + | |||
==Causes of Congenital Disorders== | ==Causes of Congenital Disorders== | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
| − | [[file:Causes.PNG| | + | [[file:Causes.PNG|500px|'''Image 1:Causes of Congenital Disorders'''|thumb]] |
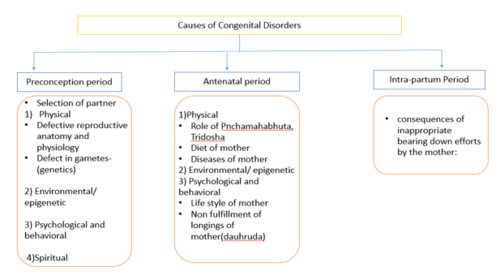
The causes of congenital disorders can be analyzed in view of physical, mental and spiritual dimensions. | The causes of congenital disorders can be analyzed in view of physical, mental and spiritual dimensions. | ||
| Line 62: | Line 65: | ||
== Factors related to preconception Period== | == Factors related to preconception Period== | ||
| + | |||
===Physical factors === | ===Physical factors === | ||
| + | |||
==== Genetic defects in parents==== | ==== Genetic defects in parents==== | ||
'''Abnormalities in gametes (beeja dosha)''' | '''Abnormalities in gametes (beeja dosha)''' | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
| − | The concept of genetics is denoted with the terms ‘beeja’(seed or gametes), ‘beejabhaga’ (chromosomes) and beeja-bhagavayava (nucleic acids and genes). The maternal (matruja) and paternal (pitruja) factors are responsible for the formation of the embryo. When any part of these three genetic materials is abnormal, it leads to deformity or mal-formation of the organ or body part. [Cha. Sa. [[Sharira Sthana]] 3/17] | + | The concept of genetics is denoted with the terms ‘beeja’(seed or gametes), ‘beejabhaga’ (chromosomes) and beeja-bhagavayava (nucleic acids and genes). The maternal (matruja) and paternal (pitruja) factors are responsible for the formation of the embryo. When any part of these three genetic materials is abnormal, it leads to deformity or mal-formation of the organ or body part. [Cha. Sa. [[Sharira Sthana]] 3/17] |
| + | |||
====Role of reproductive physiology ([[shukra dhatu]]) of parents==== | ====Role of reproductive physiology ([[shukra dhatu]]) of parents==== | ||
The vitiation of reproductive elements [[shukra dhatu]] and its channels of transformation and transportation (shukravaha srotasa) results in deformities in progeny. [Cha. Sa. [[Sutra Sthana]] 28/28], [Cha. Sa. [[Chikitsa Sthana]] 2;8/34] The normal status of [[shukra dhatu]] at the time of conception is important for normal embryogenesis. | The vitiation of reproductive elements [[shukra dhatu]] and its channels of transformation and transportation (shukravaha srotasa) results in deformities in progeny. [Cha. Sa. [[Sutra Sthana]] 28/28], [Cha. Sa. [[Chikitsa Sthana]] 2;8/34] The normal status of [[shukra dhatu]] at the time of conception is important for normal embryogenesis. | ||
| + | |||
====Disorders of female reproductive system ==== | ====Disorders of female reproductive system ==== | ||
Optimum health of uterus/female reproductive tract (kshetra) is an essential factor for the normal growth and development of the fetus. | Optimum health of uterus/female reproductive tract (kshetra) is an essential factor for the normal growth and development of the fetus. | ||
| + | |||
==== Role of time factor (kala) ==== | ==== Role of time factor (kala) ==== | ||
Age of the parents at the time of conception is important. In Ayurvedic texts, the minimum age for normal and healthy conception is described as twenty five years for male and sixteen years for female. At this age, the individual attains complete psycho-sexual maturity to become responsible parents. [Su. Sa. Sutra Sthana 35/13] Young girls and old women are not advised for conception. [Cha. Sa. [[Sharira Sthana]] 8/6] If the recommended age is not followed for conception, it can lead to intrauterine death of fetus, neonatal death, ill health and deformed body parts of the child.[A. S. Sharira Sthana 1/5] | Age of the parents at the time of conception is important. In Ayurvedic texts, the minimum age for normal and healthy conception is described as twenty five years for male and sixteen years for female. At this age, the individual attains complete psycho-sexual maturity to become responsible parents. [Su. Sa. Sutra Sthana 35/13] Young girls and old women are not advised for conception. [Cha. Sa. [[Sharira Sthana]] 8/6] If the recommended age is not followed for conception, it can lead to intrauterine death of fetus, neonatal death, ill health and deformed body parts of the child.[A. S. Sharira Sthana 1/5] | ||
Pregnancy at a very young age causes premature births. Aneuploidy (abnormal chromosome number) is the principal hereditary abnormality associated with age of either parent. Advanced maternal age is associated with increased risks for miscarriage, chromosomal abnormalities, stillbirth, foetal growth restriction and preterm birth.<ref>Frick AP. Advanced maternal age and adverse pregnancy outcomes. Best Pract Res Clin Obstet Gynaecol. 2021 Jan;70:92-100. doi: 10.1016/j.bpobgyn.2020.07.005. Epub 2020 Jul 15. PMID: 32741623.</ref>Recent research shows that younger paternal age(< 20 years) could increase the risks of urogenital abnormalities and chromosome disorders in fetus. Advanced paternal age (≥ 40 years) could increase the risks of cardiovascular abnormalities, facial deformities, urogenital abnormalities, and chromosome disorders in their offspring.<ref>Fang Y, Wang Y, Peng M, et al. Effect of paternal age on offspring birth defects: a systematic review and meta-analysis. Aging (Albany NY). 2020;12(24):25373-25394. doi:10.18632/aging.104141</ref> Growing evidences also indicate that the offspring of older fathers are prone to reduced fertility and an increased risk of birth defects, some cancers, and schizophrenia.<ref>Bray I, Gunnell D, Davey Smith G. Advanced paternal age: how old is too old?. J Epidemiol Community Health. 2006;60(10):851-853. doi:10.1136/jech.2005.045179</ref> | Pregnancy at a very young age causes premature births. Aneuploidy (abnormal chromosome number) is the principal hereditary abnormality associated with age of either parent. Advanced maternal age is associated with increased risks for miscarriage, chromosomal abnormalities, stillbirth, foetal growth restriction and preterm birth.<ref>Frick AP. Advanced maternal age and adverse pregnancy outcomes. Best Pract Res Clin Obstet Gynaecol. 2021 Jan;70:92-100. doi: 10.1016/j.bpobgyn.2020.07.005. Epub 2020 Jul 15. PMID: 32741623.</ref>Recent research shows that younger paternal age(< 20 years) could increase the risks of urogenital abnormalities and chromosome disorders in fetus. Advanced paternal age (≥ 40 years) could increase the risks of cardiovascular abnormalities, facial deformities, urogenital abnormalities, and chromosome disorders in their offspring.<ref>Fang Y, Wang Y, Peng M, et al. Effect of paternal age on offspring birth defects: a systematic review and meta-analysis. Aging (Albany NY). 2020;12(24):25373-25394. doi:10.18632/aging.104141</ref> Growing evidences also indicate that the offspring of older fathers are prone to reduced fertility and an increased risk of birth defects, some cancers, and schizophrenia.<ref>Bray I, Gunnell D, Davey Smith G. Advanced paternal age: how old is too old?. J Epidemiol Community Health. 2006;60(10):851-853. doi:10.1136/jech.2005.045179</ref> | ||
| + | |||
===Psychological and behavioral factors=== | ===Psychological and behavioral factors=== | ||
A pleasant state of mind is the prime requirement for conception. [Cha. Sa. [[Sutra Sthana]] 25/40] The mental status of parents during coitus and conception is important. Coitus shall be avoided, when either of the partners is hungry, thirsty, or frightened, averse, sorrow-stricken, angry, distressed with relationship, or not desiring for sex. These states during coitus adversely affect conception and health of progeny. [Cha. Sa. [[Sharira Sthana]] 8/17] Studies show that preconception stress alters offspring development in a parental and fetal sex-specific manner. This is reflected in the metabolic and immune-related genes in the placenta as well as brain transcriptome.<ref>Yasmine M.Cissé et al, Brain and placental transcriptional responses as a readout of maternal and paternal preconception stress are fetal sex specific, Placenta, Volume 100, October 2020, Pages 164-170.</ref> | A pleasant state of mind is the prime requirement for conception. [Cha. Sa. [[Sutra Sthana]] 25/40] The mental status of parents during coitus and conception is important. Coitus shall be avoided, when either of the partners is hungry, thirsty, or frightened, averse, sorrow-stricken, angry, distressed with relationship, or not desiring for sex. These states during coitus adversely affect conception and health of progeny. [Cha. Sa. [[Sharira Sthana]] 8/17] Studies show that preconception stress alters offspring development in a parental and fetal sex-specific manner. This is reflected in the metabolic and immune-related genes in the placenta as well as brain transcriptome.<ref>Yasmine M.Cissé et al, Brain and placental transcriptional responses as a readout of maternal and paternal preconception stress are fetal sex specific, Placenta, Volume 100, October 2020, Pages 164-170.</ref> | ||
| + | |||
===Spiritual factors === | ===Spiritual factors === | ||
| + | |||
Sinful acts and atheistic attitude of parents [Su. Sa. Sharira Sthana 2/50-52], deeds of previous life ([[atma]] –karma dosha) [Cha. Sa. [[Sharira Sthana]] 2/29] and unrighteousness(adharma) [Su. Sa. Sharira Sthana 3/36] can cause congenital disorders. These factors are commonly considered as of ‘unknown origin’ in current medical practices. | Sinful acts and atheistic attitude of parents [Su. Sa. Sharira Sthana 2/50-52], deeds of previous life ([[atma]] –karma dosha) [Cha. Sa. [[Sharira Sthana]] 2/29] and unrighteousness(adharma) [Su. Sa. Sharira Sthana 3/36] can cause congenital disorders. These factors are commonly considered as of ‘unknown origin’ in current medical practices. | ||
</div> | </div> | ||
| + | |||
==Factors related to antenatal period== | ==Factors related to antenatal period== | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
Improper antenatal care and poor nutrition during pregnancy can lead to deformity in the fetus. [Cha. Sa. [[Sharira Sthana]] 4/30] The six factors responsible for embryogenesis play an important role in the causation of congenital disorders. These include maternal (matruja), paternal (pitruja), spiritual ([[atma]]ja), psychological (sattvaja), adaptations ([[satmya]]ja) and nutritional component (rasaja). Minor defects in these factors can cause congenital abnormalities in the fetus. Major defects cause abortion or intrauterine death of the fetus. [Cha. Sa. [[Sharira Sthana]] 4/28-29] | Improper antenatal care and poor nutrition during pregnancy can lead to deformity in the fetus. [Cha. Sa. [[Sharira Sthana]] 4/30] The six factors responsible for embryogenesis play an important role in the causation of congenital disorders. These include maternal (matruja), paternal (pitruja), spiritual ([[atma]]ja), psychological (sattvaja), adaptations ([[satmya]]ja) and nutritional component (rasaja). Minor defects in these factors can cause congenital abnormalities in the fetus. Major defects cause abortion or intrauterine death of the fetus. [Cha. Sa. [[Sharira Sthana]] 4/28-29] | ||
| + | |||
===Role of [[panchamahabhuta]]=== | ===Role of [[panchamahabhuta]]=== | ||
| − | The five fundamental elements ([[pancha mahabhuta]]) play basic functions during embryogenesis. [[Vayu]] performs function of cell division/multiplication (vibhajana); [[agni]] carries function of metabolism(pachana); [[jala]] carries function of moisture or fluid (kledana); [[Prithvi]] carries function of compactness or formation of mass(samhanana); and [[akasha]] carries function of enlargement of size(vivardhana). If these functions are carried out in normal proportion, the body's normal structure (shareera) is formed. The defective proportion or functioning can adversely affect embryogenesis and result in congenital anamolies. [Su.Sa. Sharira Sthana 5/3] More specifically, [[vayu]] and [[akasha]] cause anatomical deformities in children. [Bhela Sa Sharira Sthana 3/15-16] | + | |
| + | The five fundamental elements ([[pancha mahabhuta]]) play basic functions during embryogenesis. [[Vayu]] performs function of cell division/multiplication (vibhajana); [[agni]] carries function of metabolism(pachana); [[jala]] carries function of moisture or fluid (kledana); [[Prithvi]] carries function of compactness or formation of mass(samhanana); and [[akasha]] carries function of enlargement of size(vivardhana). If these functions are carried out in normal proportion, the body's normal structure (shareera) is formed. The defective proportion or functioning can adversely affect embryogenesis and result in congenital anamolies. [Su.Sa. Sharira Sthana 5/3] More specifically, [[vayu]] and [[akasha]] cause anatomical deformities in children. [Bhela Sa Sharira Sthana 3/15-16] | ||
| + | |||
===Role of [[dosha]]=== | ===Role of [[dosha]]=== | ||
| + | |||
Vitiation of all three [[dosha]] during pregnancy can cause congenital disorders. [A. H. Sharira Sthana 1/6] [[Vata]] [[dosha]] plays key role as controller of all activities and anatomical shapes (akruti) of the embryo (garbha). [Cha. Sa. [[Sutra Sthana]] 12/8], [Su. Sa. Sharira Sthana 2/50-52] | Vitiation of all three [[dosha]] during pregnancy can cause congenital disorders. [A. H. Sharira Sthana 1/6] [[Vata]] [[dosha]] plays key role as controller of all activities and anatomical shapes (akruti) of the embryo (garbha). [Cha. Sa. [[Sutra Sthana]] 12/8], [Su. Sa. Sharira Sthana 2/50-52] | ||
| + | |||
===Role of [[ dhatu]]=== | ===Role of [[ dhatu]]=== | ||
| + | |||
The structural and functional integrity of maternal reproductive organs especially the uterus is having a great role in the growth and development of the fetus. The quality of [[rasa dhatu]] of the mother and its transportation to the fetus plays a vital role.The placenta (apara) and umbilical cord (nabhi nadi) also play crucial role in the nourishment of fetus (garbha poshana). The disorder of these structural entities certainly affects the fetus and leads to some congenital deformities. | The structural and functional integrity of maternal reproductive organs especially the uterus is having a great role in the growth and development of the fetus. The quality of [[rasa dhatu]] of the mother and its transportation to the fetus plays a vital role.The placenta (apara) and umbilical cord (nabhi nadi) also play crucial role in the nourishment of fetus (garbha poshana). The disorder of these structural entities certainly affects the fetus and leads to some congenital deformities. | ||
| + | |||
===Mental status of mother=== | ===Mental status of mother=== | ||
| + | |||
The mental status of the mother during pregnancy can influence fetal growth and development.The psychological and cognitive development of fetus depends on the psychological status of the mother and the topics listened to by the pregnant woman.[A.S. Sharira Sthana 1/66] And also, the importance of maintaining the positive psychological status of mother while treating the fetal growth related ailments like intra uterine growth restriction is being emphasized.[A.H. sharira Sthana 2/20] | The mental status of the mother during pregnancy can influence fetal growth and development.The psychological and cognitive development of fetus depends on the psychological status of the mother and the topics listened to by the pregnant woman.[A.S. Sharira Sthana 1/66] And also, the importance of maintaining the positive psychological status of mother while treating the fetal growth related ailments like intra uterine growth restriction is being emphasized.[A.H. sharira Sthana 2/20] | ||
| − | ===Diet and lifestyle of the mother | + | |
| + | ===Diet and lifestyle of the mother === | ||
| + | |||
The harmful diet and lifestyle factors followed by mothers that can adversely affect progeny (garbhopaghatakara bhavas) are described below. [Cha. Sa. [[Sharira Sthana]] 8/21] More research studies are needed to find out exact genetic connections in the causes and their effects on progeny. | The harmful diet and lifestyle factors followed by mothers that can adversely affect progeny (garbhopaghatakara bhavas) are described below. [Cha. Sa. [[Sharira Sthana]] 8/21] More research studies are needed to find out exact genetic connections in the causes and their effects on progeny. | ||
| − | ===Causes of premature birth or atrophy or emaciation of fetus | + | |
| + | ===Causes of premature birth or atrophy or emaciation of fetus === | ||
| + | |||
* Sitting in awkward positions, on uneven and hard seats | * Sitting in awkward positions, on uneven and hard seats | ||
| Line 101: | Line 125: | ||
* Excessive consumption of pungent and hot food items or less quantity of food than needed | * Excessive consumption of pungent and hot food items or less quantity of food than needed | ||
| − | ===Causes of miscarriage | + | |
| + | ===Causes of miscarriage === | ||
| + | |||
* Repeated trauma or injuries, looking down from heights (e.g., from mountain-tops or cliffs, deep wells, etc.) | * Repeated trauma or injuries, looking down from heights (e.g., from mountain-tops or cliffs, deep wells, etc.) | ||
| Line 107: | Line 133: | ||
* Prolong exposure to loud and unpleasant noise | * Prolong exposure to loud and unpleasant noise | ||
| − | ===Causes of mental retardation and psychiatric disorders in child | + | |
| + | ===Causes of mental retardation and psychiatric disorders in child === | ||
| + | |||
* Excess sleeping in open air or walking at night leads to the birth of a mentally challenged child. | * Excess sleeping in open air or walking at night leads to the birth of a mentally challenged child. | ||
| Line 120: | Line 148: | ||
* A woman who is a thief will give birth to a lazy child who is wicked and inept. | * A woman who is a thief will give birth to a lazy child who is wicked and inept. | ||
| − | * An intolerant woman would give birth to a child who is of fierce, deceitful, and jealous nature. | + | * An intolerant woman would give birth to a child who is of fierce, deceitful, and jealous nature. |
| − | ===Lifestyle-related causes | + | |
| + | ===Lifestyle-related causes === | ||
| + | |||
* A woman who sleeps for long hours would give birth to a dull and unwise child with poor digestive capacity. | * A woman who sleeps for long hours would give birth to a dull and unwise child with poor digestive capacity. | ||
* A woman addicted to wines gives birth to a child who is ever-thirsty and fickle-minded. | * A woman addicted to wines gives birth to a child who is ever-thirsty and fickle-minded. | ||
| − | ===Dietary causes | + | |
| + | ===Dietary causes === | ||
| + | |||
* A woman who consumes flesh and meat of godha (iguana) would give birth to a child afflicted with stones or shanairmeha (a type of urinary disorder where dribbling is seen) | * A woman who consumes flesh and meat of godha (iguana) would give birth to a child afflicted with stones or shanairmeha (a type of urinary disorder where dribbling is seen) | ||
| Line 149: | Line 181: | ||
A systematic review shows that parental alcohol exposures are significantly associated with the risk of congenital heart diseases in offspring. This highlights the necessity of improving health awareness to prevent alcohol exposure during preconception and conception periods.<ref>Zhang S, Wang L, Yang T, Chen L, Zhao L, Wang T, Chen L, Ye Z, Zheng Z, Qin J. Parental alcohol consumption and the risk of congenital heart diseases in offspring: An updated systematic review and meta-analysis. Eur J Prev Cardiol. 2020 Mar;27(4):410-421. doi: 10.1177/2047487319874530. Epub 2019 Oct 2. PMID: 31578093.</ref> | A systematic review shows that parental alcohol exposures are significantly associated with the risk of congenital heart diseases in offspring. This highlights the necessity of improving health awareness to prevent alcohol exposure during preconception and conception periods.<ref>Zhang S, Wang L, Yang T, Chen L, Zhao L, Wang T, Chen L, Ye Z, Zheng Z, Qin J. Parental alcohol consumption and the risk of congenital heart diseases in offspring: An updated systematic review and meta-analysis. Eur J Prev Cardiol. 2020 Mar;27(4):410-421. doi: 10.1177/2047487319874530. Epub 2019 Oct 2. PMID: 31578093.</ref> | ||
| + | |||
===Effect of maternal diseases upon the fetus=== | ===Effect of maternal diseases upon the fetus=== | ||
| − | The affliction of the body part of the pregnant woman, either by vitiation of [[dosha ]] or trauma, leads to the affliction of the identical part of the fetal body. [ Su. Sa. Sharira Sthana 3/17] Maternal autoantibodies can cross the placenta and cause fetal damage. For example, fetal thyroid goiter can be developed in response to maternal Graves' disease.<ref>Panaitescu AM, Nicolaides K. Maternal autoimmune disorders and fetal defects. J Matern Fetal Neonatal Med. 2018;31(13):1798‐1806. doi:10.1080/14767058.2017.1326904</ref> | + | |
| − | ===Effect of non-fulfillment of longings/desires of the mother during pregnancy (dauhruda vimanana) | + | The affliction of the body part of the pregnant woman, either by vitiation of [[dosha ]] or trauma, leads to the affliction of the identical part of the fetal body. [ Su. Sa. Sharira Sthana 3/17] Maternal autoantibodies can cross the placenta and cause fetal damage. For example, fetal thyroid goiter can be developed in response to maternal Graves' disease.<ref>Panaitescu AM, Nicolaides K. Maternal autoimmune disorders and fetal defects. J Matern Fetal Neonatal Med. 2018;31(13):1798‐1806. doi:10.1080/14767058.2017.1326904</ref> |
| + | |||
| + | ===Effect of non-fulfillment of longings/desires of the mother during pregnancy (dauhruda vimanana)=== | ||
| + | |||
The fetus expresses desires through mother. Hence the desires of the pregnant woman (dauhruda) should always be fulfilled. Any negligence or non-fulfillment can cause abnormalities or even death of the fetus. Suppression of desires vitiates [[vayu]], and produces various diseases, abnormalities in the fetus, or even death. [Cha. Sa. [[Sharira Sthana]] 4/25] | The fetus expresses desires through mother. Hence the desires of the pregnant woman (dauhruda) should always be fulfilled. Any negligence or non-fulfillment can cause abnormalities or even death of the fetus. Suppression of desires vitiates [[vayu]], and produces various diseases, abnormalities in the fetus, or even death. [Cha. Sa. [[Sharira Sthana]] 4/25] | ||
| − | Various studies indicate that mental illness and neurocognitive decline are prevalent co-morbidities in the adolescent and adult population with congenital heart diseases (CHD).<ref>Khanna AD, Duca LM, Kay JD, Shore J, Kelly SL, Crume T. Prevalence of Mental Illness in Adolescents and Adults With Congenital Heart Disease from the Colorado Congenital Heart Defect Surveillance System. Am J Cardiol. 2019;124(4):618‐626. doi:10.1016/j.amjcard.2019.05.023</ref> <ref>Keir M, Ebert P, Kovacs AH, et al. Neurocognition in Adult Congenital Heart Disease: How to Monitor and Prevent Progressive Decline. Can J Cardiol. 2019;35(12):1675‐1685. doi:10.1016/j.cjca.2019.06.020 </ref> | + | Various studies indicate that mental illness and neurocognitive decline are prevalent co-morbidities in the adolescent and adult population with congenital heart diseases (CHD).<ref>Khanna AD, Duca LM, Kay JD, Shore J, Kelly SL, Crume T. Prevalence of Mental Illness in Adolescents and Adults With Congenital Heart Disease from the Colorado Congenital Heart Defect Surveillance System. Am J Cardiol. 2019;124(4):618‐626. doi:10.1016/j.amjcard.2019.05.023</ref> <ref>Keir M, Ebert P, Kovacs AH, et al. Neurocognition in Adult Congenital Heart Disease: How to Monitor and Prevent Progressive Decline. Can J Cardiol. 2019;35(12):1675‐1685. doi:10.1016/j.cjca.2019.06.020 </ref> |
| + | |||
=== Environmental factors=== | === Environmental factors=== | ||
| + | |||
Environmental conditions can play a role in fetal development. A retrospective cohort study reported a significant positive association between soil cadmium and air pollution evaluated by air quality index (AQI) and level of screening serum TSH in congenital hypothyroidism patients. It is inferred that the interaction of genetic, autoimmune, familial, and environmental factors with each other could have an influence on neonatal thyroid function.<ref>Hashemipour, M., Kelishadi, R., Amin, M.M. et al. The association between familial and environmental factors and prevalence of congenital hypothyroidism in center of Iran. Environ Sci Pollut Res (2020). https://doi.org/10.1007/s11356-020-10959-x</ref> | Environmental conditions can play a role in fetal development. A retrospective cohort study reported a significant positive association between soil cadmium and air pollution evaluated by air quality index (AQI) and level of screening serum TSH in congenital hypothyroidism patients. It is inferred that the interaction of genetic, autoimmune, familial, and environmental factors with each other could have an influence on neonatal thyroid function.<ref>Hashemipour, M., Kelishadi, R., Amin, M.M. et al. The association between familial and environmental factors and prevalence of congenital hypothyroidism in center of Iran. Environ Sci Pollut Res (2020). https://doi.org/10.1007/s11356-020-10959-x</ref> | ||
</div> | </div> | ||
| + | |||
==Factors related to intra partum period== | ==Factors related to intra partum period== | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
| Line 162: | Line 201: | ||
If bearing down efforts are made in the absence of real labour pains, deafness, dumbness, dislocation of mandible, head and neck diseases, cough, dyspnoea, emaciation, and abnormal location of the body parts of the child are likely to occur. [ Su. Sa. Sharira Sthana 10/9] | If bearing down efforts are made in the absence of real labour pains, deafness, dumbness, dislocation of mandible, head and neck diseases, cough, dyspnoea, emaciation, and abnormal location of the body parts of the child are likely to occur. [ Su. Sa. Sharira Sthana 10/9] | ||
</div> | </div> | ||
| − | ==Classification of congenital disorders | + | |
| + | ==Classification of congenital disorders == | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
The congenital disorders are classified in two major categories. [ Su. Sa. Sutra Sthana 24/5] | The congenital disorders are classified in two major categories. [ Su. Sa. Sutra Sthana 24/5] | ||
| Line 203: | Line 243: | ||
The following table shows comprehensive information about genetic disorders and their consequences on progeny. | The following table shows comprehensive information about genetic disorders and their consequences on progeny. | ||
| + | |||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 221: | Line 262: | ||
Some genetic conditions are caused by mutations in only a single gene. These conditions are usually inherited in different patterns, depending on the type of gene. | Some genetic conditions are caused by mutations in only a single gene. These conditions are usually inherited in different patterns, depending on the type of gene. | ||
| + | |||
The following table shows some examples. | The following table shows some examples. | ||
| + | |||
{| class="wikitable" | {| class="wikitable" | ||
|- | |- | ||
| Line 279: | Line 322: | ||
==Diagnosis of Congenital disorders== | ==Diagnosis of Congenital disorders== | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
| − | ===History of parents | + | ===History of parents=== |
A careful history of either several spontaneous abortions or offspring with multiple anomalies is an indication for chromosome analyses on both parents. Among known genetic disorders, the severity of X-linked disorders differs in males and females. Genetic mutations originate more frequently among males, and the frequency increases with advancing paternal age. This is seen in Marfan syndrome, achondroplasia, hemophilia A, and the Lesch-Nyhan syndrome.<ref>Congenital deformities and chromosomal disorders: maternal versus paternal age. Fertil Steril. 1977;28(8):888. doi:10.1016/s0015-0282(16)42748-2</ref> | A careful history of either several spontaneous abortions or offspring with multiple anomalies is an indication for chromosome analyses on both parents. Among known genetic disorders, the severity of X-linked disorders differs in males and females. Genetic mutations originate more frequently among males, and the frequency increases with advancing paternal age. This is seen in Marfan syndrome, achondroplasia, hemophilia A, and the Lesch-Nyhan syndrome.<ref>Congenital deformities and chromosomal disorders: maternal versus paternal age. Fertil Steril. 1977;28(8):888. doi:10.1016/s0015-0282(16)42748-2</ref> | ||
| Line 296: | Line 339: | ||
An anomaly scan or mid-pregnancy scan is done to detect significant physical abnormalities in the growing baby. It is an ultrasound scan done between the 18th and 21st week of pregnancy. It helps detect congenital disorders like anencephaly, diaphragmatic hernia, gastroschisis, exomphalos, open spina bifida, bilateral renal agenesis, lethal skeletal dysplasia, Edwards’ syndrome or T18, Patau’s syndrome or T13, cleft lip and serious cardiac abnormalities.<ref>Available from https://www.motherhoodindia.com/specialities-pregnancy-care/pregnancy-scans/anomaly-scan-detail/ cited on 17/06/2021 </ref> | An anomaly scan or mid-pregnancy scan is done to detect significant physical abnormalities in the growing baby. It is an ultrasound scan done between the 18th and 21st week of pregnancy. It helps detect congenital disorders like anencephaly, diaphragmatic hernia, gastroschisis, exomphalos, open spina bifida, bilateral renal agenesis, lethal skeletal dysplasia, Edwards’ syndrome or T18, Patau’s syndrome or T13, cleft lip and serious cardiac abnormalities.<ref>Available from https://www.motherhoodindia.com/specialities-pregnancy-care/pregnancy-scans/anomaly-scan-detail/ cited on 17/06/2021 </ref> | ||
| − | ===Clinical examination | + | ===Clinical examination=== |
Clinical diagnosis of congenital disorders is based on the three-fold diagnostic tools. | Clinical diagnosis of congenital disorders is based on the three-fold diagnostic tools. | ||
| Line 306: | Line 349: | ||
'''3) Interrogation (prashna):''' The detailed history of both the parents regarding the family history, personal history, medical history should be taken to rule out or to find the cause of a congenital disorder in the child. It can be useful in diagnosis and prevention of hereditary disorders. | '''3) Interrogation (prashna):''' The detailed history of both the parents regarding the family history, personal history, medical history should be taken to rule out or to find the cause of a congenital disorder in the child. It can be useful in diagnosis and prevention of hereditary disorders. | ||
</div> | </div> | ||
| + | |||
==Treatment == | ==Treatment == | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
| Line 319: | Line 363: | ||
In other skin changes, which are circular in shape, covering a large or small area, bluish black or white in colour (known as nyaccha), bloodletting therapy (sira vyadha) as per convenience is advised. [Su. Sa. Chikitsa Sthana 20/33] | In other skin changes, which are circular in shape, covering a large or small area, bluish black or white in colour (known as nyaccha), bloodletting therapy (sira vyadha) as per convenience is advised. [Su. Sa. Chikitsa Sthana 20/33] | ||
</div> | </div> | ||
| + | |||
==Preventive aspects of congenital disorders== | ==Preventive aspects of congenital disorders== | ||
<div style="text-align:justify;"> | <div style="text-align:justify;"> | ||
Pre-conception guidelines are recommended for healthy progeny and to prevent congenital disorders. The guidelines include the selection of partners, purification procedures, and prenatal care. | Pre-conception guidelines are recommended for healthy progeny and to prevent congenital disorders. The guidelines include the selection of partners, purification procedures, and prenatal care. | ||
| − | ===Guidelines for selection of partner | + | ===Guidelines for selection of partner=== |
The selection of a partner with desirable qualities is the prime step in the prevention of congenital disorders. The following are the guidelines for the selection of an ideal partner as per Ayurveda text. | The selection of a partner with desirable qualities is the prime step in the prevention of congenital disorders. The following are the guidelines for the selection of an ideal partner as per Ayurveda text. | ||
| Line 346: | Line 391: | ||
===Preventive and therapeutic protocol=== | ===Preventive and therapeutic protocol=== | ||
| + | |||
If either the parents or both of them have any hereditary disorders, the therapies are advised. [[Panchakarma]] procedures including therapeutic purgation ([[virechana]]) followed by administration of [[rasayana]] and [[vajikarana]] therapy can help to prevent or minimize genetic disorders in progeny. Suppose the first child is born with any kind of congenital disorder. In that case, the preventive protocol must be followed before planning for the next baby. | If either the parents or both of them have any hereditary disorders, the therapies are advised. [[Panchakarma]] procedures including therapeutic purgation ([[virechana]]) followed by administration of [[rasayana]] and [[vajikarana]] therapy can help to prevent or minimize genetic disorders in progeny. Suppose the first child is born with any kind of congenital disorder. In that case, the preventive protocol must be followed before planning for the next baby. | ||
</div> | </div> | ||
| Line 393: | Line 439: | ||
Avaleha, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. | Avaleha, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. | ||
| − | 10. Anjana A. goswami ( 2015) A clinical study on Beejadushtijanya pandu | + | 10. Anjana A. goswami ( 2015) : A clinical study on Beejadushtijanya pandu |
(Thalasemia major) and its management with Gandhakadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. | (Thalasemia major) and its management with Gandhakadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. | ||
| − | 11. O.T.M.R. Senani B kalawana (2016 ) | + | 11. O.T.M.R. Senani B kalawana (2016 ) : Management of Beejadushtijanya pandu(Thalasemia major) with Musta-triphladi avaleha and gandhkadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. |
| − | 12. Rahul Gameti (2017) Further clinical study on Beejadushtijanya pandu | + | 12. Rahul Gameti (2017): Further clinical study on Beejadushtijanya pandu |
(Thalasemia major)and its management with Gandhakadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. | (Thalasemia major)and its management with Gandhakadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar. | ||
| Line 405: | Line 451: | ||
==More information == | ==More information == | ||
| − | |||
| − | [[Khuddika Garbhavakranti Sharira]] | + | [[ Atulyagotriya Sharira]] , [[Khuddika Garbhavakranti Sharira]], [[Mahatigarbhavakranti Sharira]], [[ Jatisutriya Sharira ]], [[Yonivyapat Chikitsa Adhyaya]], [[Garbha]], [[Prenatal care (garbhini paricharya)]] |
| − | [[ | + | <big>'''[[Special:ContactMe|Send us your suggestions and feedback on this page.]]'''</big> |
| − | + | ==References== | |
| − | == | + | <div id="BackToTop" class="noprint" style="background-color:#DDEFDD; position:fixed; |
| + | bottom:32px; left:2%; z-index:9999; padding:0; margin:0;"><span style="color:blue; | ||
| + | font-size:8pt; font-face:verdana,sans-serif; border:0.2em outset #ceebf7; | ||
| + | padding:0.1em; font-weight:bolder; -moz-border-radius:8px; "> | ||
| + | [[#top| Back to the Top ]]</span></div> | ||
Revision as of 00:26, 24 September 2021
Understanding congenital disorders in Ayurveda and contemporary research
Congenital disorders are disabilities or malformations present at or before birth. These are identified in prenatal life or at birth, or many years later. As per the World Health Organization, congenital anomalies are a leading cause of neonatal deaths. Every year an estimated 295 000 newborns die within 28 days of birth due to congenital anomalies. These can contribute to long-term disability, with significant impacts on individuals, families, healthcare systems, and societies. [1]
Human genetics studies individual genes, their role and function in disease, and their mode of inheritance. Genomics refers to an organism's entire genetic information, the genome,and the function and interaction of DNA within the genome, as well as with environmental or nongenetic factors such as a person's lifestyle. Characterization of the human genome in genomic studies has supported genetics to elucidate the etiology, pathogenesis of the disease, and improve therapeutic interventions and outcomes. The impressive advances in genetics, genomics, and health care information technology have significantly increased the wealth of knowledge. It is helpful in medical practice and play a prominent role in the diagnosis, prevention, and treatment of disease.[2] The ancient rishis of Ayurveda had recognized the genetic basis of diseases. They have documented the knowledge in various contexts. The current medical system focuses on the identification of genes responsible for diseases. At the same time, the references found in Ayurveda texts indicate the causes of genetic disorders and their role in health and diseases. A proper study to bridge the gaps and connect these two pools of information can reveal significant insights for a comprehensive understanding of why and what of congenital and genetic disorders. The present article describes congenital disorders in Ayurveda texts and contemporary research.
| Section/Chapter/topic | Sharira / Garbha / Congenital disorders |
|---|---|
| Authors | Anagha S.1, Deole Y.S.1 |
| Reviewers | Basisht G.1, Chavan- Gautam P.2 |
| Editor | Basisht G.1 |
| Affiliations |
1Charak Samhita Research, Training and Development Centre, I.P.G.T.& R.A., Jamnagar, 2 Center for Complementary & Integrative Health, Savitribai Phule Pune University, Maharashtra, India. |
| Correspondence email | carakasamhita@gmail.com |
| Date of first publication: | July 21, 2021 |
| DOI | Under process |
Congenital disorders as per Ayurveda
In Ayurveda, the congenital disorders are considered incurable(asadhya) with poor prognosis. Similarly, some hereditary of familial (kulaja) ailments are also explained as incurable.
E.g. Congenital or hereditary obstinate urinary diseases including diabetes (Jataja prameha) [Cha. Sa. Chikitsa Sthana 6/57]
Ayurveda emphasizes on prevention of congenital disorders through proper preconception, ante- natal and intra partum care. The causes for congenital disorders are explained in detail. These are helpful in taking necessary actions to avoid such risk factors and obtaining a healthy progeny.
Causes of Congenital Disorders
The causes of congenital disorders can be analyzed in view of physical, mental and spiritual dimensions.
These causes can be broadly classified based on period:
1) Preconception period
2) Antenatal period
3) Intra-partum period
Physical factors
Genetic defects in parents
Abnormalities in gametes (beeja dosha)
The concept of genetics is denoted with the terms ‘beeja’(seed or gametes), ‘beejabhaga’ (chromosomes) and beeja-bhagavayava (nucleic acids and genes). The maternal (matruja) and paternal (pitruja) factors are responsible for the formation of the embryo. When any part of these three genetic materials is abnormal, it leads to deformity or mal-formation of the organ or body part. [Cha. Sa. Sharira Sthana 3/17]
Role of reproductive physiology (shukra dhatu) of parents
The vitiation of reproductive elements shukra dhatu and its channels of transformation and transportation (shukravaha srotasa) results in deformities in progeny. [Cha. Sa. Sutra Sthana 28/28], [Cha. Sa. Chikitsa Sthana 2;8/34] The normal status of shukra dhatu at the time of conception is important for normal embryogenesis.
Disorders of female reproductive system
Optimum health of uterus/female reproductive tract (kshetra) is an essential factor for the normal growth and development of the fetus.
Role of time factor (kala)
Age of the parents at the time of conception is important. In Ayurvedic texts, the minimum age for normal and healthy conception is described as twenty five years for male and sixteen years for female. At this age, the individual attains complete psycho-sexual maturity to become responsible parents. [Su. Sa. Sutra Sthana 35/13] Young girls and old women are not advised for conception. [Cha. Sa. Sharira Sthana 8/6] If the recommended age is not followed for conception, it can lead to intrauterine death of fetus, neonatal death, ill health and deformed body parts of the child.[A. S. Sharira Sthana 1/5]
Pregnancy at a very young age causes premature births. Aneuploidy (abnormal chromosome number) is the principal hereditary abnormality associated with age of either parent. Advanced maternal age is associated with increased risks for miscarriage, chromosomal abnormalities, stillbirth, foetal growth restriction and preterm birth.[3]Recent research shows that younger paternal age(< 20 years) could increase the risks of urogenital abnormalities and chromosome disorders in fetus. Advanced paternal age (≥ 40 years) could increase the risks of cardiovascular abnormalities, facial deformities, urogenital abnormalities, and chromosome disorders in their offspring.[4] Growing evidences also indicate that the offspring of older fathers are prone to reduced fertility and an increased risk of birth defects, some cancers, and schizophrenia.[5]
Psychological and behavioral factors
A pleasant state of mind is the prime requirement for conception. [Cha. Sa. Sutra Sthana 25/40] The mental status of parents during coitus and conception is important. Coitus shall be avoided, when either of the partners is hungry, thirsty, or frightened, averse, sorrow-stricken, angry, distressed with relationship, or not desiring for sex. These states during coitus adversely affect conception and health of progeny. [Cha. Sa. Sharira Sthana 8/17] Studies show that preconception stress alters offspring development in a parental and fetal sex-specific manner. This is reflected in the metabolic and immune-related genes in the placenta as well as brain transcriptome.[6]
Spiritual factors
Sinful acts and atheistic attitude of parents [Su. Sa. Sharira Sthana 2/50-52], deeds of previous life (atma –karma dosha) [Cha. Sa. Sharira Sthana 2/29] and unrighteousness(adharma) [Su. Sa. Sharira Sthana 3/36] can cause congenital disorders. These factors are commonly considered as of ‘unknown origin’ in current medical practices.
Improper antenatal care and poor nutrition during pregnancy can lead to deformity in the fetus. [Cha. Sa. Sharira Sthana 4/30] The six factors responsible for embryogenesis play an important role in the causation of congenital disorders. These include maternal (matruja), paternal (pitruja), spiritual (atmaja), psychological (sattvaja), adaptations (satmyaja) and nutritional component (rasaja). Minor defects in these factors can cause congenital abnormalities in the fetus. Major defects cause abortion or intrauterine death of the fetus. [Cha. Sa. Sharira Sthana 4/28-29]
Role of panchamahabhuta
The five fundamental elements (pancha mahabhuta) play basic functions during embryogenesis. Vayu performs function of cell division/multiplication (vibhajana); agni carries function of metabolism(pachana); jala carries function of moisture or fluid (kledana); Prithvi carries function of compactness or formation of mass(samhanana); and akasha carries function of enlargement of size(vivardhana). If these functions are carried out in normal proportion, the body's normal structure (shareera) is formed. The defective proportion or functioning can adversely affect embryogenesis and result in congenital anamolies. [Su.Sa. Sharira Sthana 5/3] More specifically, vayu and akasha cause anatomical deformities in children. [Bhela Sa Sharira Sthana 3/15-16]
Role of dosha
Vitiation of all three dosha during pregnancy can cause congenital disorders. [A. H. Sharira Sthana 1/6] Vata dosha plays key role as controller of all activities and anatomical shapes (akruti) of the embryo (garbha). [Cha. Sa. Sutra Sthana 12/8], [Su. Sa. Sharira Sthana 2/50-52]
Role of dhatu
The structural and functional integrity of maternal reproductive organs especially the uterus is having a great role in the growth and development of the fetus. The quality of rasa dhatu of the mother and its transportation to the fetus plays a vital role.The placenta (apara) and umbilical cord (nabhi nadi) also play crucial role in the nourishment of fetus (garbha poshana). The disorder of these structural entities certainly affects the fetus and leads to some congenital deformities.
Mental status of mother
The mental status of the mother during pregnancy can influence fetal growth and development.The psychological and cognitive development of fetus depends on the psychological status of the mother and the topics listened to by the pregnant woman.[A.S. Sharira Sthana 1/66] And also, the importance of maintaining the positive psychological status of mother while treating the fetal growth related ailments like intra uterine growth restriction is being emphasized.[A.H. sharira Sthana 2/20]
Diet and lifestyle of the mother
The harmful diet and lifestyle factors followed by mothers that can adversely affect progeny (garbhopaghatakara bhavas) are described below. [Cha. Sa. Sharira Sthana 8/21] More research studies are needed to find out exact genetic connections in the causes and their effects on progeny.
Causes of premature birth or atrophy or emaciation of fetus
- Sitting in awkward positions, on uneven and hard seats
- Suppressing the urge to pass flatus, urine, and defecation
- Indulgence in intensive or extreme forms of physical activities
- Excessive consumption of pungent and hot food items or less quantity of food than needed
Causes of miscarriage
- Repeated trauma or injuries, looking down from heights (e.g., from mountain-tops or cliffs, deep wells, etc.)
- Traveling long distances in excessively jerky carriages
- Prolong exposure to loud and unpleasant noise
Causes of mental retardation and psychiatric disorders in child
- Excess sleeping in open air or walking at night leads to the birth of a mentally challenged child.
- Indulgence in too many quarrels and fights can lead to epilepsy in a child.
- Excess indulgence in coitus (or a nymphomaniac) leads to the birth of a truant with a passion for women.
- Constant grief in pregnancy would give birth to a timid, or under-developed, or short-lived child.
- A woman who always thinks ill of others gives birth to a delinquent or an anti-social child.
- A woman who is a thief will give birth to a lazy child who is wicked and inept.
- An intolerant woman would give birth to a child who is of fierce, deceitful, and jealous nature.
- A woman who sleeps for long hours would give birth to a dull and unwise child with poor digestive capacity.
- A woman addicted to wines gives birth to a child who is ever-thirsty and fickle-minded.
Dietary causes
- A woman who consumes flesh and meat of godha (iguana) would give birth to a child afflicted with stones or shanairmeha (a type of urinary disorder where dribbling is seen)
- A woman who consumes pork frequently would give birth to a child with red eyes, rough body-hair, and prone to suffering from severe respiratory disorders.
- A woman who used to consume fish excessively would give birth to a child with lagophthalmos and related eye disorders
- A woman used to eating many sweets is prone to giving birth to a dumb or excessively obese child or a diabetic child.
- A woman fond of sour food items is prone to giving birth to an offspring suffering from bleeding disorders or diseases of the skin and eyes.
- A woman who consumes more salt or salty food articles may give birth to a child with early onset of wrinkles, grey hair, or baldness.
- A woman used to pungent substances in excess may give birth to a weak child, deficient in semen and impotent.
- A woman using bitter substances in excess may give birth to a child with emaciated, weak or undeveloped body.
- A woman habituated to excessive use of astringents may give birth to a child with a blackish complexion, suffering from constipation and udavarta (misperistalsis).
[Cha.Sa. Sharira Sthana 8/21]
The effect of diet taken by the mother vitiating particular dosha is described. [A. S. Sharira Sthana 2/54-56]
A systematic review shows that parental alcohol exposures are significantly associated with the risk of congenital heart diseases in offspring. This highlights the necessity of improving health awareness to prevent alcohol exposure during preconception and conception periods.[7]
Effect of maternal diseases upon the fetus
The affliction of the body part of the pregnant woman, either by vitiation of dosha or trauma, leads to the affliction of the identical part of the fetal body. [ Su. Sa. Sharira Sthana 3/17] Maternal autoantibodies can cross the placenta and cause fetal damage. For example, fetal thyroid goiter can be developed in response to maternal Graves' disease.[8]
Effect of non-fulfillment of longings/desires of the mother during pregnancy (dauhruda vimanana)
The fetus expresses desires through mother. Hence the desires of the pregnant woman (dauhruda) should always be fulfilled. Any negligence or non-fulfillment can cause abnormalities or even death of the fetus. Suppression of desires vitiates vayu, and produces various diseases, abnormalities in the fetus, or even death. [Cha. Sa. Sharira Sthana 4/25] Various studies indicate that mental illness and neurocognitive decline are prevalent co-morbidities in the adolescent and adult population with congenital heart diseases (CHD).[9] [10]
Environmental factors
Environmental conditions can play a role in fetal development. A retrospective cohort study reported a significant positive association between soil cadmium and air pollution evaluated by air quality index (AQI) and level of screening serum TSH in congenital hypothyroidism patients. It is inferred that the interaction of genetic, autoimmune, familial, and environmental factors with each other could have an influence on neonatal thyroid function.[11]
Consequences of inappropriate bearing down efforts by the mother: If bearing down efforts are made in the absence of real labour pains, deafness, dumbness, dislocation of mandible, head and neck diseases, cough, dyspnoea, emaciation, and abnormal location of the body parts of the child are likely to occur. [ Su. Sa. Sharira Sthana 10/9]
Classification of congenital disorders
The congenital disorders are classified in two major categories. [ Su. Sa. Sutra Sthana 24/5]
1) Due to genetic defects (aadibalapravrutta):
These include maternal (matruja) or paternal (pitruja) genetic factors. These can be termed as ‘pre-conception causes’.
Examples:
- Skin lesions (kushtha): Skin lesions resembling the petal of lotus(pundarika), fruit of Abrus pricatorius (kakanaka)[Su. Sa. Nidana Sthana 5/19] and congenital skin patches of different size, shape and colour.[Su. Sa. Nidana Sthana 13/41-44]
- Hemorrhoids (arsha)[ Su. Sa. Sutra Sthana 24/5]
- Obstinate urinary disorders (prameha)[ Su. Sa. Sutra Sthana 24/5]
- Emaciation (karshya/kshaya) [Dalhana, Su. Sa. Sutra Sthana 24/5]
- Shandi yoni vyapad (female without sexual desire and undeveloped breasts) is caused due to abnormalities in male and female gametes (beeja dosha) and affliction of the uterus by vitiated vata dsoha. [Cha. Sa. Chikitsa Sthana 30/34-35] This condition is similar to the chromosomal disorder known as “Turner’s syndrome”.
- The defects in the sperm (shukra) cause deformities in factors related to paternal origin. [Cha. Sa. Sharira Sthana 4/30-31]
2) Disorders due to faulty diet and lifestyle habits of mother, especially during the prenatal period (janmabalapravrutta):
These may be either due to nutritional factors (rasakruta) or psychological factors (duahruda apacharakruta). These can be termed as ‘post-conception causes’.
Examples:
- Limb deformities (pangu)
- Congenital blindness (jatyandhya)
- Deafness (badhira)
- Dumbness (mooka)
- Nasal voice (minmina)
- Dwarfism (vaamana)
The following table shows comprehensive information about genetic disorders and their consequences on progeny.
| Gender | Vitiated factor | Outcome | Possible modern co-relation |
|---|---|---|---|
| Female | Genes in maternal chromosomes(beejabhaga of shonita), responsible for the formation of uterus(garbhashaya) | female not capable of reproduction, infertile female(vandhya) | Agenesis of uterus/adnexa leading to infertility |
| Female | Some of the DNA bases (beejabhaga avayava) in the genes of maternal chromosomes responsible for the formation of uterus (garbhashaya) | can conceive, but deliver only dead fetus (putipraja) | Recurrent pregnancy loss due to genetic disorders. |
| Female | Some of the DNA bases(beejabhaga avayva) in the genes of maternal chromosomes responsible for the formation of uterus (garbhashaya) as well as those responsible for developing feminine characters | incomplete female/ transgender (varta) | Gonadal dysgenesis Eg:-Turner Syndrome,Swyer Syndrome |
| Male | Genes in paternal chromosomes(beejabhaga of shukra), responsible for the formation of sperms(shukra) | sterile male (vandhya) | Male Infertility due gonadal agenesis |
| Male | Some of the DNA bases(beejabhaga avayva) in the genes of paternal chromosomes responsible for the formation of sperms(shukra) | offspring dies after delivery (putipraja) | Recurrent pregnancy loss due to genetic disorders |
| Male | Some of the DNA bases (beejabhaga avayava) in the genes of paternal chromosomes responsible for the formation of sperms(shukra) as well as those responsible for developing masculine characters. | incomplete male /transgender (trinaputrika) | Gonadal dysgenesis |
Some genetic conditions are caused by mutations in only a single gene. These conditions are usually inherited in different patterns, depending on the type of gene.
The following table shows some examples.
| Pattern of inheritance | Description | Example |
|---|---|---|
| X-linked dominant | *By mutations in genes on the X chromosome,
|
fragile X syndrome |
| X-linked recessive | * Caused by mutations in genes on the X chromosome.
|
hemophilia, Fabry disease |
| Y-linked | * Caused by mutations in genes on the Y chromosome.
|
Y chromosome infertility, some cases of Swyer syndrome |
| Autosomal dominant | * One mutated copy of the gene in each cell is sufficient for a person to be affected.
|
Huntington disease, Marfan syndrome |
| Autosomal recessive | * Both copies of the gene in each cell should have mutations.
|
cystic fibrosis, sickle cell disease |
| Codominant | * Two different versions (alleles) of a gene are expressed.
|
ABO blood group, alpha-1 antitrypsin deficiency |
| Mitochondrial | * Also known as maternal inheritance
|
Leber hereditary optic neuropathy (LHON) |
Many health conditions are caused by the combined effects of multiple genes which are known as polygenic. It may be by the interactions between genes and the environment also. For example, heart disease, type 2 diabetes, schizophrenia, certain types of cancer etc.[12]
Diagnosis of Congenital disorders
History of parents
A careful history of either several spontaneous abortions or offspring with multiple anomalies is an indication for chromosome analyses on both parents. Among known genetic disorders, the severity of X-linked disorders differs in males and females. Genetic mutations originate more frequently among males, and the frequency increases with advancing paternal age. This is seen in Marfan syndrome, achondroplasia, hemophilia A, and the Lesch-Nyhan syndrome.[13] The genetic analyses in such cases can diagnose probable genetic disorders in progeny.
Check up before pregnancy:
The genetic diseases like cystic fibrosis, fragile X syndrome, sickle cell disease, Tay-Sachs disease, Spinal muscular atrophy can be identified in carrier parents before pregnancy. It can also be done in high-risk category parents who are susceptible to disorders due to ethnicity. Common susceptible groups that may be carriers include non-Hispanic whites (cystic fibrosis), people of Eastern European Jewish descent (Tay-Sachs disease, cystic fibrosis, and others), and those of African, Mediterranean, and Southeast Asian backgrounds (sickle cell disease). [14]
During pregnancy:
The risk of Down syndrome, trisomy 18, and spine and brain problems can be diagnosed between 10 and 13 weeks of pregnancy by check up. The cell free fetal DNA testing, AFP (alphafetoprotein) test, Maternal serum quad screen, Amniocentesis and Chorionic Villus Sampling (CVS) are done in susceptible cases.
Antenatal anomaly scan:
An anomaly scan or mid-pregnancy scan is done to detect significant physical abnormalities in the growing baby. It is an ultrasound scan done between the 18th and 21st week of pregnancy. It helps detect congenital disorders like anencephaly, diaphragmatic hernia, gastroschisis, exomphalos, open spina bifida, bilateral renal agenesis, lethal skeletal dysplasia, Edwards’ syndrome or T18, Patau’s syndrome or T13, cleft lip and serious cardiac abnormalities.[15]
Clinical examination
Clinical diagnosis of congenital disorders is based on the three-fold diagnostic tools.
1) Inspection (darshana): A careful neonatal examination after birth can identify visible structural deformities. The examination findings in each part of the neonate body for the signs which indicate life span. [Cha. Sa. Sharira Sthana 8/51]
2) Palpation (sparshana): Any structural deformity or anatomical abnormality can be easily detected by palpation. [Cha. Sa. Sharira Sthana 8/43], [A.Hr. Uttara Sthana 1/1]
3) Interrogation (prashna): The detailed history of both the parents regarding the family history, personal history, medical history should be taken to rule out or to find the cause of a congenital disorder in the child. It can be useful in diagnosis and prevention of hereditary disorders.
Treatment
Most of congenital disorders are incurable. The patients shall be well informed about the prognosis before treating such diseases. The measures to minimize the symptoms of the particular disorder and improve the quality of life should be the goal of treatment.
Surgical procedures:
Some surgical or para surgical measures are advised in case of minor structural deformities like Stricture of uretra (nirudha prakasha)[Su. Sa. Nidana Sthana 13/52-54] and imperforate anus (sannirudha gudam) [Su. Sa. Nidana Sthana 13/55-56]. The description of the surgical procedure is also available for the treatment of these congenital disorders.[Su. Sa. Chikitsa Sthana 20/43-47]
In congenital skin patches that are small,round, painless, slightly raised, light red coloured and smooth (known as jatumani), blackish, minute as in sesame seed size (tilakalaka)etc. cauterization using caustic alkali(kshara karma) or thermal cauterization (agnikarma) is advised.[Su. Sa. Chikitsa Sthana 20/32]
In other skin changes, which are circular in shape, covering a large or small area, bluish black or white in colour (known as nyaccha), bloodletting therapy (sira vyadha) as per convenience is advised. [Su. Sa. Chikitsa Sthana 20/33]
Preventive aspects of congenital disorders
Pre-conception guidelines are recommended for healthy progeny and to prevent congenital disorders. The guidelines include the selection of partners, purification procedures, and prenatal care.
Guidelines for selection of partner
The selection of a partner with desirable qualities is the prime step in the prevention of congenital disorders. The following are the guidelines for the selection of an ideal partner as per Ayurveda text.
- The partner should belong to a different clan (gotra).[ Cha. Sa. Sharira Sthana 2/3]
- Consanguinity in sexual relationships should be avoided.
- Either partner should not have any hereditary disorders or familial traits.
- Either partner should not be suffering from any contagious or sexually transmitted diseases.
- Either partner should not be handicapped.
- Both should possess attractive physical characters.
- Both partners should be healthy and follow good health habits.
- Both should follow good morals and conduct. [A. S. Sharira Sthana 1/3]
These guidelines are essential to prevent the transmission of genetic disorders in the family.
Preventive and therapeutic protocol
If either the parents or both of them have any hereditary disorders, the therapies are advised. Panchakarma procedures including therapeutic purgation (virechana) followed by administration of rasayana and vajikarana therapy can help to prevent or minimize genetic disorders in progeny. Suppose the first child is born with any kind of congenital disorder. In that case, the preventive protocol must be followed before planning for the next baby.
Current research
Contemporary approach:
As per modern embryology, susceptibility to teratogenesis depends on the genotype of the conceptus and the manner in which this genetic composition interacts with the environment. The maternal genome is also important with respect to drug metabolism, resistance to infection, and other biochemical and molecular processes that affect the conceptus. Susceptibility to teratogens varies with the developmental stage at the time of exposure.
The most sensitive period for inducing congenital disabilities is the third to eight weeks of gestation, the period of embryogenesis.[16]
There are three phases of intrauterine growth. Zygote, embryo, and fetus.
1. The zygote phase or Period-I (weeks 1 – 2 after fertilization): It consists of cell division and implantation of this cell mass in the uterus. During this phase, teratogen would cause loss of the conceptus.
2. The embryonic phase or Period II (weeks 3 – 8): In this period, most of the organ systems develop. This is the most vulnerable phase for major congenital malformations to occur.
3. The fetal phase / Period III (weeks 9 – 38): In this phase, further growth and elaboration of the organ systems take place. During this phase, various factors can result in minor or not-so-severe defects.
Congenital disabilities occur due to three main reasons i.e.abnormal formation of tissues, abnormal forces on normal tissues, or destruction of normal tissues. Some of these defects may have a cascade effect and result in related anomalies or multiple anomalies (syndromes).[17]
Nowadays, allogeneic hematopoietic stem cell transplantation (allo-HSCT) is emerging as a treatment of choice for various congenital disorders.[18]
Theses works done
1. M.N. Jaiswal (2003): Clinical role of indigenous drugs (Amalaki Rasayana and Gomeda Bhasma) in Kulaja Pandu (Thalassemia)-A scientific study, Dept. of Kaumarabhrutya., Shree Ayurved Mahavidhyalaya, Nagpur.
2. Ruchi Singh (2007): A study of disease Thalassemia (Anukta Vyadhi Ayurveda) and its management with Dhatri Avaleha, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
3. Jadhav Sahebrao B (2009): A study of disease Thalassemia (Anukta Vyadhi in Ayurveda) and its management with Triphaladi Avaleha as an adjuvant therapy, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
4. Joban K. Modha (2009): A comparative pharmaco-pharmaceutical clinical study of Gandhakadi Yoga B on Iron overloading condition due to Raktavikruti, Deprtment of RSBK, I.PG.T & R.A, Jamnagar.
5. Pramod R. Yadav (2010): The pharmaceutical standardization of Gandhakadi Yoga and its effect on Thalassemic iron overload w.s.r. to Kadli as pathya, Deprtment of RSBK, I.PG.T & R.A, Jamnagar.
6. Sagar Nalawade (2011): Pharmacological study of Amritasara Lohokta Dosha Nivaraka Dravya on iron overloading with special reference to Thalassemia Major, NIA, Jaipur.
7. Abhishek Y. Patalia (2011): A study of Beejadushtijanya Pandu and its management with Triphaladi Avaleha w.s.r. to Thalassemia, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
8. Raina Rathod (2013): A further clinical study on Beejadushtijanya Pandu- Thalassemia Major and with Triphaladi Avaleha, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
9. Shailesh R. Rajgolkar (2014): A clinical study on Beejadushtijanya pandu (Thalassemia major) in children and its management with Musta-Triphaladi Avaleha, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
10. Anjana A. goswami ( 2015) : A clinical study on Beejadushtijanya pandu (Thalasemia major) and its management with Gandhakadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
11. O.T.M.R. Senani B kalawana (2016 ) : Management of Beejadushtijanya pandu(Thalasemia major) with Musta-triphladi avaleha and gandhkadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
12. Rahul Gameti (2017): Further clinical study on Beejadushtijanya pandu (Thalasemia major)and its management with Gandhakadi yoga, Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
13. Bhumi Mori(2018) : Management of Beejadushtijanya Pandu (Thalassemia Major) with modified Musta-Triphaladi Avaleha and Gandhakadi Yoga: An Open Labelled, Randomized, Controlled, Clinical Trial , Department of Kaumarabhrutya, I.PG.T & R.A, Jamnagar.
More information
Atulyagotriya Sharira , Khuddika Garbhavakranti Sharira, Mahatigarbhavakranti Sharira, Jatisutriya Sharira , Yonivyapat Chikitsa Adhyaya, Garbha, Prenatal care (garbhini paricharya)
Send us your suggestions and feedback on this page.
References
- ↑ Available from https://www.who.int/news-room/fact-sheets/detail/congenital-anomalies accessed on 15/06/2021
- ↑ J. Larry Ja meson, Peter Kopp. Principles of Human Genetics. In Harrison’s principles of internal medicine. 19th edition. Pg. 425.
- ↑ Frick AP. Advanced maternal age and adverse pregnancy outcomes. Best Pract Res Clin Obstet Gynaecol. 2021 Jan;70:92-100. doi: 10.1016/j.bpobgyn.2020.07.005. Epub 2020 Jul 15. PMID: 32741623.
- ↑ Fang Y, Wang Y, Peng M, et al. Effect of paternal age on offspring birth defects: a systematic review and meta-analysis. Aging (Albany NY). 2020;12(24):25373-25394. doi:10.18632/aging.104141
- ↑ Bray I, Gunnell D, Davey Smith G. Advanced paternal age: how old is too old?. J Epidemiol Community Health. 2006;60(10):851-853. doi:10.1136/jech.2005.045179
- ↑ Yasmine M.Cissé et al, Brain and placental transcriptional responses as a readout of maternal and paternal preconception stress are fetal sex specific, Placenta, Volume 100, October 2020, Pages 164-170.
- ↑ Zhang S, Wang L, Yang T, Chen L, Zhao L, Wang T, Chen L, Ye Z, Zheng Z, Qin J. Parental alcohol consumption and the risk of congenital heart diseases in offspring: An updated systematic review and meta-analysis. Eur J Prev Cardiol. 2020 Mar;27(4):410-421. doi: 10.1177/2047487319874530. Epub 2019 Oct 2. PMID: 31578093.
- ↑ Panaitescu AM, Nicolaides K. Maternal autoimmune disorders and fetal defects. J Matern Fetal Neonatal Med. 2018;31(13):1798‐1806. doi:10.1080/14767058.2017.1326904
- ↑ Khanna AD, Duca LM, Kay JD, Shore J, Kelly SL, Crume T. Prevalence of Mental Illness in Adolescents and Adults With Congenital Heart Disease from the Colorado Congenital Heart Defect Surveillance System. Am J Cardiol. 2019;124(4):618‐626. doi:10.1016/j.amjcard.2019.05.023
- ↑ Keir M, Ebert P, Kovacs AH, et al. Neurocognition in Adult Congenital Heart Disease: How to Monitor and Prevent Progressive Decline. Can J Cardiol. 2019;35(12):1675‐1685. doi:10.1016/j.cjca.2019.06.020
- ↑ Hashemipour, M., Kelishadi, R., Amin, M.M. et al. The association between familial and environmental factors and prevalence of congenital hypothyroidism in center of Iran. Environ Sci Pollut Res (2020). https://doi.org/10.1007/s11356-020-10959-x
- ↑ https://ghr.nlm.nih.gov/primer/inheritance/inheritancepatterns
- ↑ Congenital deformities and chromosomal disorders: maternal versus paternal age. Fertil Steril. 1977;28(8):888. doi:10.1016/s0015-0282(16)42748-2
- ↑ Available from https://www.webmd.com/baby/pregnant-genetic-testing cited on 17/06/2021
- ↑ Available from https://www.motherhoodindia.com/specialities-pregnancy-care/pregnancy-scans/anomaly-scan-detail/ cited on 17/06/2021
- ↑ Prof.Hari Hirdya Awasthi,Dr.Mohd.Ashraf Khan, Garbha sarira, Chaukhambha Orientalia. Varanasi; 1996. First edition.pg.136
- ↑ Dhiman K, Kumar A, Dhiman KS. Shad Garbhakara Bhavas vis-a-vis congenital and genetic disorders. Ayu. 2010;31(2):175‐184. doi:10.4103/0974-8520.72384
- ↑ Faraci M, Giardino S, Bagnasco F, et al. Allogeneic hematopoietic stem cell transplantation in congenital disorders: A single-center experience. Pediatr Transplant. 2017;21(6):10.1111/petr.12997. doi:10.1111/petr.12997