Difference between revisions of "Amavata"
| Line 131: | Line 131: | ||
'''Symbiohealth approach:''' | '''Symbiohealth approach:''' | ||
| − | [[File:Simbiohealth.JPG|500px|'''Figure 1: Symbiohealth approach [Source: AYU Journal]'''|thumb]] | + | [[File:Simbiohealth.JPG|500px|'''Figure 1: Symbiohealth approach [Source: Basisht et.al. AYU Journal]'''|thumb]] |
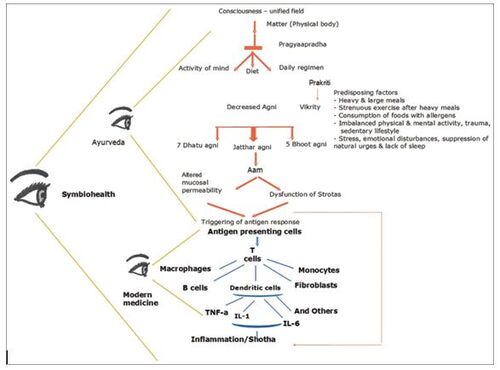
Symbiohealth approach focuses on comprehensive management of disease by including offence and defence strategies of management. A comparative study of the pathogenesis and treatment of RA according to modern medicine and Ayurveda gives many insights helpful in the management of this potentially crippling disease [Figure 1]. It broadens the horizon to win the war against disease. This approach depends upon severity and stage of disease. | Symbiohealth approach focuses on comprehensive management of disease by including offence and defence strategies of management. A comparative study of the pathogenesis and treatment of RA according to modern medicine and Ayurveda gives many insights helpful in the management of this potentially crippling disease [Figure 1]. It broadens the horizon to win the war against disease. This approach depends upon severity and stage of disease. | ||
Simbiohealth.JPG | Simbiohealth.JPG | ||
Revision as of 06:28, 18 August 2021
The clinical condition in which aggravated vata is associated with metabolic toxins (ama) and mainly affects joints is termed as ‘amavata’. This condition closely resembles with rheumatoid arthritis. The main culprit behind this disease is the deranged digestion and metabolism (agni). Arthralgia, stiffness and swellings of joint are main clinical features. The treatment is focused to improve digestion and metabolism and maintain equilibrium of vata dosha. Detail description of amavata as a separate disease entity is observed in the text of Madhava Nidana.
A comparative study of the pathophysiology of this disease by Ayurveda and allopathic system reveals that modern medicine emphasizes on control of inflammation with use of NSAIDS, immunosuppressants and TNF blockers. This is an “offence strategy” which has rapid response but needs to be continued indefinitely and has high incidence of toxicity. On the other hand Ayurveda follows primarily a “defense strategy” which takes longer time to control inflammation and the symptoms but incidence of toxicity is very little, if at all. In patients with acute inflammation and severe discomfort, initial treatment should be with immunosuppressants and TNF blockers. On control of acute symptoms ayurvedic treatment should be continued. This combined (Symbiohealth) approach in the management of disease can give insight into the genetic and epigenetic phenomenon and opens the doors for groundbreaking research.[1] This article describes the etiopathogenesis and management of amavata.
National Ayurveda Morbidity Code: EC-6
ICD code: M06.9
Keywords: Amavata, rheumatoid arthritis, ama, basti, niruha, ruksha sweda
| Section/Chapter/topic | Chikitsa / Vyadhi / Amavata |
|---|---|
| Authors | Aneesh E.G., Deole Y.S. |
| Reviewed by | Basisht G. |
| Affiliations | Charak Samhita Research, Training and Development Centre, I.T. R.A., Jamnagar |
| Correspondence email: | carakasamhita@gmail.com |
| Date of first publication: | August 18, 2021 |
| DOI | In process |
Causes (hetu)
- Dietary: Intake of incompatible combinations of foods. [M.Ni 25/01][2], irregular dietary habits.
- Lifestyle: Indulging in strenuousactivities immediately after intake of unctuous/heavy to digest foods. [M.Ni 25/01][2]
- Psychological: Negative mental states while taking meals. [Cha.Sa. Vimana Sthana 2/9 ] Stress is a triggering factor for rheumatoid arthritis.[3]
- Others: Improper management in pregnancy and post partum period causing aggravation of vata can lead to amavata.[4]
Clinical features
General clinical features
Body ache, anorexia, morbid thirst, laziness, heaviness, feverishness, indigestion and edema in body parts are the general features of amavata in its initial phase. [M.Ni 25/6][2] When the disease aggravates, it causes severe pain associated with swelling especially in joints of upper and lower limbs and in sacral region. Generalized symptoms like loss of appetite, pain or heaviness in abdomen, excessive micturition, burning sensation, sleep disturbances, constipation, abdominal distention, vomiting, giddiness are also seen. [M.Ni.25/7-10][2]
Dosha specific clinical features
| Dosha | Specific clinical features |
|---|---|
| Vata | Pain |
| Pitta | Burning sensation and reddish discoloration |
| Kapha | Rigidity, heaviness and itching |
Pathogenesis
Continuous use of incompatible foods and indulging in strenuous activities immediately after unctuous meal leads to indigestion. The channels of transportation and transformation of body fluid (rasavaha srotasa) and marrow (majjavaha srotas) are affected by incompatible foods. This leads to the formation of ama (metabolic toxins). These toxins are circulated all over the body by vyana vata.
Physical exercise after taking food is crucial cause of amavata. This is responsible for the movement of dosha from gastrointestinal tract (koshta) to peripheral tissues (shakha). The circulating toxins accumulate in the joints and affect the associated structures at the joint. This causes clinical features of amavata.[5]
In amavata, the intestinal mucosal permeability and peristalsis is impaired. Alteration of bacterial flora of the gut occurs. These factors may result in malabsorption. This causes indigestion and further vitiation of dosha.[6]
Thus, the pathogenesis (samprapti) of amavata begins with the impairment of agni (digestion and metabolism) in the gastrointestinal tract. It further extends to vital organs, bones and joints (madhyama rogamarga) with a special affinity towards natural sites of kapha dosha, especially joints (sandhi).[7]
Predisposing and contributing factors
- Heavy and large meals in relation to digestive fire or Agni.
- Strenuous exercise or physical activity after a heavy meal.
- Consumption of food with allergens, e.g., animal products, nuts, wheat products, and seafood.
- Imbalanced physical activity based upon the body type, trauma on the one hand and sedentary life-style on the other.
- Inflammatory bowel disease.
- Stress, emotional disturbances, suppression of natural urges, and lack of sleep.
Clinical diagnosis
The diagnosis of amavata is based on observation of clinical features. The gradation of clinical features is done to assess the severity of the disease.
Biomarkers for diagnosis and assessment of efficacy
Rheumatoid arthritis factor, Erythrocyte sedimentation rate (ESR)[8], Anti-cyclic citrullinated peptides (Anti CCP)[4], C-reactive protein (CRP)[9] are used to diagnose the condition of rheumatoid arthritis.
Prognosis
| Clinical feature | Prognosis |
|---|---|
| If involvement of only one dosha | Curable |
| If involvement of two dosha | Palliable (yapya) |
| If involvement of all dosha, Presence of generalized edema | Difficult to treat |
[M.Ni.25/12][2]
Management
Stage wise management of disease
I. Acute condition:
The acute condition of amavata is managed in allopathic system by anti-inflammatory agents like non steroidal anti inflammatory drugs (NSAIDs), disease modifying agents, biological agents like TNF blockers and surgery. This offence strategy is useful to relive pain and decrease inflammation in short term management of acute conditions.
II. Chronic condition:
When the disease is in chronic stage, the quality of tissues is depleted. Thus the defence mechanism is weak. The treatment objective is focused to strengthen the defence mechanism and manage the aggravating factors. The defence strategy includes restoring equilibrium of dosha and agni, clearing channels by removing ama and thereafter enhancing strength of tissues.
Symbiohealth approach:
Symbiohealth approach focuses on comprehensive management of disease by including offence and defence strategies of management. A comparative study of the pathogenesis and treatment of RA according to modern medicine and Ayurveda gives many insights helpful in the management of this potentially crippling disease [Figure 1]. It broadens the horizon to win the war against disease. This approach depends upon severity and stage of disease. Simbiohealth.JPG
Preventive strategies
Following disease specific wholesome diet and liefestyle can prevent the occurance as well as recurrence of disease. The regimen of pathya-apathya (wholesome and unwholesome regimen) are useful in reducing the drug dependence, dosage and duration of treatment.
Wholesome foods or Pathya
- Warm water medicated with Panchkola (Pippali, Pippalimula, Chavya, Chitraka, Shunthi) in small quantity at a time helps in digestion and disintegration of Aama.
- Barley, horse gram, kodo millet and the red variety of rice are recommended. These foods are light and easy to digest. Barley kernels and other products made from barley lower inflammatory markers.
- Green leafy vegetables and fruits contain a variety of polyphenols, bioflavonoids, catechins, carotenoids, vitamin C, riboflavin, vitamin E, and low molecular weight compounds. These constituents have antioxidant, fibrinolytic and anti-inflammatory characteristics. Vegetables preferably with bitter taste like bitter melon (Memordica charantia), Neem (Azadirachta indica), Patola or luffa, Gokharu (Tribulus terrestris) are recommended.
- Spices like ginger, turmeric and garlic help to add flavor to these dishes and also have antimicrobial, anti-inflammatory and analgesic properties besides their Agni promoting impact.
- Wine-old wine, Asava and Arishta.
- Meat of Laav Pakshi-Jungle bush quail (Perdicula asiatica) prepared with traditional buttermilk.[10], [11]
Wholesome lifestyle
- Following proper daily regimen (dinacharya) and night regimen (ratricharya)
- Yogic exercise in the morning time
- Breathing exercise (pranayama)
- Meditation
Foods to avoid or Apathya
The majority of allergens come from dairy and animal products, which cause an increased production of pro-inflammatory prostaglandins.
- Cold and impure water
- Lentils like Urad and heavy foods.
- Vegetable like arabi or eddo (Colocacia antiquorum), Indian spinach (Basella rubra).
- Fish and sea foods.
Unwholesome lifestyle
- Strenous physical activities after taking heavy meals
- Stress, emotional disturbances, suppression of natural urges, and lack of sleep.
- Daytime sleep after meals.
Principles of management
The principles of management of amavata are focused on following:
- Correcting the digestion and metabolism (agni)
- Correcting the ama status of dosha
- Preventing the formation of ama
- Restoring the impaired intestinal mucosa and bacterial flora [6]
Following therapies are applied to treat amavata
- Therapeutic fasting (langhana)
- Dry fomentation (swedana)
- Use of appetizers (deepana)
- Use of foods and drugs with bitter and pungent taste
- Therapeutic purgation (virechana)
- Therapeutic enema (basti)
[Chakradatta Amavatachikitsa][12]
Currently used important herbs
Piper longum (pippali): In a study 73 clinically diagnosed Rheumatoid arthritis patients were administered powder of Piper longum (pippali) in increasing dose pattern. Initially, on first day 1 gm of Piper longum (pippali) powder twice a day with honey was given. The dose was increased daily by 1gm upto 5gm twice a day. The 5gm dose (maximum dose) was maintained for 5 days. Then the dose was tapered by 1 gm daily upto 1gm twice a day. After this, mild purgation with castor oil was given. The pain, stiffness, swelling and movement restriction in joints decreased significantly by 50.56%, 48.57%, 53.22% and 46.43% respectively. A significant reduction in ESR was also reported after this treatment. Pippali leads to digestion of accumulated toxic metabolic toxins (ama) by its stimulating (deepana) and appetizer activity. It also has rejuvenating (rasayana) and immunomodulating actions.[13]
Allium sativum (rasona): A study on 63 patients of rheumatoid arthritis (amavata), was conducted to compare the efficacy of a polyherbal formulation of Allium sativum (rasonapinda), with nucoxia (Cox-2 inhibitor Etoricoxib) as a standard control drug used for the treatment of arthritis. Three months of treatment with rasonapinda showed significant reduction in pain, swelling, stiffness and tenderness. There was significant reduction in CRP and RA titer. Allium sativum (rasona) is reported to have anti-inflammatory action. Allicin and alliinase, alkaloids present in rasona is proved effective in treating rheumatoid arthritis. Another ingredient, curcuma longa also has anti-inflammatory actions. Curcumin present in curcuma is having anti-inflammatory, anti-arthritic and anti-rheumatic properties. Rasonapinda might have prostaglandin synthesis inhibition action which results in reduced secretion of prostaglandins. The reduction in pain may be due to the decreased PGE2 release into the joint space. Reduction in swelling in joints might be due to the inhibition of IL-6, IL-1 and TNF alpha. Reduction in IL-6 might also be the cause for reduction in ESR levels.[14]
Asteracantha longifolia (kokilaksha) is found to effective in treating rheumatoid arthritis. Its anti-inflammatory property is already reported. The higher protein content may help to enhance the immunity. It may also help to destruct the immune aggregate, which is one of the basic causes for the disease.[15]
Tinospora cordifolia (guduchi), Zingiber officinale (shunthi), Semecarpus anacardium (bhallataka) are also usedbased on clinical conditions. [Chikitsapradeepa Amavataroga][16] Shunthi possess active principles gingerol, dehydrozingerone and gingerdione. These are potent prostaglandin inhibitors. Thus, it attains anti – arthritic effect. Glycosides present in Guduchi acts like NSAIDs thus producing anti – arthritic effect.[17]
Currently used important herbal formulations
If the condition is associated with fever, Amrutottaram kwatha, Amritarishta and Chitrakasava are used.[18]
Decoctions:
MahaRasnadikwatha, Ashwagandharistha, RasnaPanchakKwatha, RasnaSaptakaKwatha, Dashamoolarishta, and Amritarishta.
Herbal powder mixtures/Churnas:
Ajmodadi Churna, Panchakol Churna, Shunthi Churna, Ashwagandha Churna, Dashamool Churna, Rasna Churna, Musta Churna, Vaishwanara Churna.
Tablets:
Simhanad Guggulu, Mahayogaraja Guggulu, Yogaraja Guggulu, Punarnava Guggulu, Triphala Guggulu.
Ghee/Oil:
Panchakola Ghrita, Rasnadi Ghrita, Ashwagandha Ghrita, Dashamula Taila, Eranda Taila (castor oil), Narayana Taila, Dhanvantara Taila.
Avaleha:
Bhallataka Avaleha, Gorakha Avaleha.
Various preparations of Bhallataka can be used in Aamavata. However, these preparations shall be used with precaution in case of dominance of pitta dosha.
Research on ayurvedic formulations
Rasonarasnadighanavati, Simhanadaguggulu: In a study, 101 amavata patients were divided into two groups. In one group Rasonarasnadighanavati (250mg) was administered in the dosage of 2 tablets three times a day with hot water for 3 months. In addition to this,rasonarasnadilepa was applied at the affected joints twice a day for three months. In another group, simhanadaguggulu was administered in the dose of 2 tablets thrice a day with hot water for 3 months. General signs and symptoms of amavata were reduced in both the groups. Rasonarasnadighanavati showed better pain reliving action. Simhanadaguggulu showed better reduction in swelling of joints. Most of the drugs in rasonarasnadighanavati possess pungent and bitter taste, hot potency, rasayana and ama digesting properties. This helps to break the disease pathogenesis. Moreover, it has immunomodulatory action too. Simhanadaguggulu possess vata-kapha pacifying action and stimulates digestive capacity. It has antioxidant properties also.[5] Bitter and pungent taste, hot potency, dry and light properties of the drugs help to break the pathogenesis. All these properties are antagonistic to ama and vata. Kindling the digestive capacity helps to correct the ama status and there by removes the obstruction in the channels.[19]
In an experimental study, rheumatoid arthritis was induced in male wister rats. A formulation containing Commifora mukul, Strychnosnux vomica, Boswellia sereta, Maharasnadi kwatha and Suvarna bhasma was administered. It was found effective in reducing the signs and symptoms of Rheumatoid arthritis. These drugs have proven anti-inflammatory activity. The active principles like guggulsterones, boswellic acid, brucine can inhibit inflammatory mediator over production.[20]
Vatari guggulu: A study on 58 patients diagnosed with amavata reported vatari guggulu is effective in reducing the symptoms such as pain, swelling, stiffness and tenderness in joints. There was statistically significant reduction in RA factor,too. However, the study showed the efficacy of drug decreases with increase in the chronicity of disease.[9] The general symptoms like bodyache, heaviness, anorexia were significantly reduced significantly by vatari guggulu.[21]
Alambushadi Ghana vati: Alambushadi ghana vati is observed effective in reducing the pain, stiffness, swelling and tenderness associated with amavata. There was 60% reduction in anorexia and more than 66% reduction in fever.[22]
Amrita ghrita: A study conducted on 28 patients of amavata patients reported that administration of amrita ghrita is helpful in managing the signs and symptoms of amavata. There was 43% reduction in ESR, 51% reduction in ASO titer and CRP reduced by 63% after 45 days of administration of 15 gm of amrita ghrita with milk.[17]
Rasnerandadi kwatha[18],Rasnasaptaka kwatha, Rasnapanchaka kwatha, Rasnadashamula kwatha, Yogaraja guggulu, Vaishwanara churna are also mentioned for the treatment of amavata. [Chakradatta][12]
Currently used important herbo-mineral formulations
If associated with fever: Amavatari rasa, Vettumaran gulika[18]
Panchakarma procedures with safety precautions
Therapeutic enema (basti)
Panchamuladi basti: In a study, 12 patients having rheumatoid arthritis (amavata) were managed with Ayurvedic treatment protocol. It included initial 3 days of fasting followed by 3 days of deepana and pachana therapy with 10gm trikatu powder 3 times a day with hot water after food. This is followed by 15 days of therapeutic enema (basti) schedule. Here the schedule of basti includes 2 medicated unctuous enema (anuvasana basti) initially, 5 decoction enema (niruha basti) and 5 medicated unctuous enema (anuvasana basti) intermittently and 5 medicated unctuous enema (anuvasana basti) in the end. Panchamuladi basti is used as niruha and panchamuladi taila is used for anuvasana. There were highly significant results in disease specific symptoms like pain in joints, swelling, stiffness, warmth and tenderness in joints. Highly significant results were also seen in general symptoms like heaviness (gaurava), malaise (angamarda), indigestion (apaka), edema (angashunata) and laziness (alasya). Total 70% reduction in thirst and a complete recovery from feverishness were also reported. The alkaline nature of this basti cures the ama along with it controls the vata dosha also. Unctuous enema also helps to control vata dosha by acting directly over the main site of vata that is colon (pakwashaya).[7]
Alambushadi basti: In a study conducted on 64 patients of amavata, it is reported that the treatment protocol including Alambushadi basti and Alambushadi powder is highly effective in managing amavata. The treatment protocol consists of langhana for 3 days followed by deepana and pachana therapy with panchakola churna and chitrakadi vati respectively for 3 days. In chronic patients, abhyanga with saindhavadi taila was done for 15 days. The 15 ml of erandataila with luke warm milk was given at bed time for 7 days. For next 8 days, basti was administered. After the completion of basti, Alambushadi churna was given in the dose of 3gm thrice a day for 15 days with warm water. This protocol is found very effective in reducing pain, swelling, tenderness and stiffness associated with amavata. Reduction was also seen in RA factor and CRP titer. Amrita (tinospora cordifolia), an ingredient of alambushadi compound is proven anti-rheumatic, anti-inflammatory and immune stimulant drug. It is having rasayana and tridosha pacifying action. Tribulus terrestris (gokshura) and Crateva religiosa (varuna) pacify vata and kapha dosha.They have diuretic action that helps in reducing the swelling. Zingiber officinale (shunthi) is hot in potency and corrects the metabolism. It improves digestive power there by digests the ama.[23]
Balaguduchyadi decoction enema: Significant relief in pain and stiffness associated with Ankylosing spondylitis was reported after the administration of enema with Balaguduchyadi decoction.[18]
Kshara basti: A study conducted on 50 amavata patients, kshara basti as decoction enema followed by unctuous enema with castor oil was found effective in reducing the pain and swelling in joints, anorexia and generalized body ache. There was significant reduction in ESR and RA factor.[8]
Vaitarana basti: Vaitarana basti with its sharply acting, hot, light and dry properties increases digestion and metabolism. It reduces accumulation of toxic biological waste products (ama). Vaitarana basti along with disease pacifying oral medication is reported to be highly effective in reducing the signs and symptoms of amavata. There was 78% reduction in pain, reduction in swelling was 73% and 81% improvement in joint movements. There was highly significant reduction in ESR.[22]
Therapeutic purgation (virechana): Purgation especially with castor oil is indicated in amavata [Chikitsa pradeepa][16] Recinolic acid present in castor oil acts as purgative and it helps to scavenge remove the free radicals from body.[9]
Fomentation (swedana): Fomentation especially in dry form is indicated in amavata. For e.g. Fomentation using sand bolus. [Chakradatta][12]
Wholesome diet and lifestyle factors
- Diet has an important role in pathogenesis, prevention and management of amavata. In auto immune disorders like RA when compared with healthy individuals, there is a marked shift in intestinal microbiota and reduced commensal gut microbial community. The wholesome diet act over gut microbiota in RA patients. Immune boosting and synthesis of short chain fatty acids (SCFAs) from food plays an important role in the status of gut microbiota too.
- Anti-inflammatory activity against auto immune disorders is seen in Bowman Birk inhibitor (BBI), a proteinase inhibitor present in horse gram (kulattha). Barley (yava) increases the levels of Bifidobacterium species and lactobacillus species, which belongs to healthy gut microbiomes. Garlic increases the healthier gut bacteria and helps in maintaining the equilibrium of gut microbiota by protecting them from intestinal inflammation. Gingerols, the active principle present in ginger has the capacity to inhibit the inflammatory responses. The polyphenols present in Moringa oleifera has ability to modify the gut microbial composition. It arrests the development of pathogenic bacteria like Escherichia coli. At the same time it promotes the growth of probiotics like lactobacillus. Buttermilk is a natural probiotic diet due to presence of abundant healthy gut bacteria. The probiotics after reaching the intestine digests the dietary fibres and forms SCFAs.[24]
- The treatment of amavata includes use of diet with bitter and pungent taste. They are rich source of tannins and bioflavonoids, that are powerful anti-oxidants and have free radical scavenging property.[6]
Case reports and research updates
A diagnosed case of Ankylosing spondylitis was treated according to the treatment principles of amavata. A 21 years old male patient complaining of severe pain in low back and both knee joints with morning stiffness for more than an hour. Intermittent fever with chills and headache were also present. Reduced appetite and constipation was associated complaints. The investigations like ESR was 140 mm/hr, MRI of lumbar spine suggested bilateral sacrolitis and Human leukocyte antigen (HLA B27) was positive. The diagnosis of amavata was made based on clinical features. Initially to reduce the fever, Amrutotaram kwata, Amavatari rasa and Amritarishta were given. Since the fever persists after two weeks Amavatari rasa and Amritarishta were replaced with Vettumaran gulika and Chitrakasava. After the subsidence of fever lepa was applied over the painful areas with Kottamchukkadi churna and dhanyamla. Swelling and pain in joint subsides but since the patient develops skin rashes kottamchukkadi was replace with Grihadumadi churna. After 1 month the patient was able to walk without support and the fever subsided completely. Then the internal medications were revised to Indukantam kwatha, Marmagulika and Shaddharana churna. Fomentation with bolus of Kolakulathadi powder was also applied for 10 days. Therapeutic purgation (virechana) with Gandharvaeranda was administered on alternate days. After fomentation, pain in low back and other joints was reduced. Morning stiffness was still present. Therapeutic enema (basti) was administered in kala basti pattern. It included six balaguduchyadi niruha basti and 9 anuvasana basti. Significant improvement in pain and stiffness was noticed after the basti. Niruha basti is the main treatment for rheumatic disorders. After that as pacifying therapy Rasna-erandadi kwata, Simhanada guggulu and Gandharva-eranda was administered. His ESR was reduced to 5mm/hr after 3 months of treatment.[18]
A 27 year old female patient developed amavata, 1 month after her delivery. She complaints of pain and swelling in bilateral corpo-phalangel joints, both knees and ankles along with morning stiffness, anorexia and bodyache for six months. Tenderness along with raised body temperature and stiffness was present in the affected joints. Her RA factor and Anti CCP antibody were positive. RA factor 160 IU/ml and anti CCP more than 200 units/ml. Patient was treated with oral medications and panchakarma treatments. During the entire course of treatment, she continued breast feeding and the baby showed normal growth and development. The treatment for four months includes oral administration of Simhanada guggulu, Pratapalankeshwara rasa, Dashamoolakatutraya kashaya, combination of Swarnabhupati rasa, mahavatavidhvansa rasa, Tapyadiloha along with Smilax china (chopachini), Zinziber officinale (shunthi) and Tinospora cordifolia (guduchi). Panchakarma treatment includes whole body massage with Vishagharbhataila, fomentation in wooden chamber (bashpa sweda) and therapeutic enema (basti). The basti schedule consists of total 16 basti, including 10 unctuous enema and 6 decoction enema. For unctuous enema, 60 ml Pippalyadi taila, 10ml honey and 3gm rock salt were used. For decoction enema, 500ml decoction is prepared with dashamoola etc. drugs with paste (100ml) of tamarind and jaggery, 100ml cow’s urine, 40 ml Pippalyaditaila, 30ml honey and 5 gm rock salt. After the panchakarma treatment patient continued the oral medications and application of Vishagarbha taila for three months. There was marked reduction in bodyache and anorexia after the first 15 days of treatment but morning stiffness persists. After 1 month of panchakarma treatment, morning stiffness reduced. After 75 days of treatment, there was considerable reduction in tenderness and edema in joints and complete subsidence of anorexia and bodyache. After 4 months of treatment, the patient become completely symptom free and RA factor came to normal level. Pratapalankeshwara rasa is beneficial in reducing vata especially in postpartum stage. Dasamoolakatutraya pacifies vata, improves digestion, nourishes blood and is having the ability to reduce the pain in joints. Swarnabhupati rasa acts on vatakapha disorders related with musculoskeletal system. Tapyadiloha improves blood, Chopachini, shunthi and guduchi digests the ama and clears the obstruction in the path of vata.[4]
A 54 yearold woman diagnosed as Rheumatoid arthritis associated with hypertension and type 2 diabetes was reported to be treated through an integrative approach which includes Naturopathy, Yoga and Acupuncture. The patient complains of moderate to severe pain, swelling and morning stiffness in multiple joints especially over bilateral small joints, elbow, shoulder, knees and hip. Hydrotherapy, mud therapy, massage therapy, yoga therapy and acupuncture were given for 10 days as a supportive treatment. There was improvement in pain, ESR, FBS, PPBS counts. These therapies are reported to have analgesic action. Mud therapy may reduce the inflammation. Sulphur minerals present in mud might get absorbed through skin results in analgesic effect. The action over thermo and mechano receptors through hydro therapy may block nociceptors there by reducing pain. Muscle relaxation achieved through massage might be the cause for pain reduction through massage therapy. Pain reduction through acupuncture might be through modulation of nor adrenaline and serotonin signalling system. Formation of endogenous opioids, somatostatin and other neurotrophins may block the passage of pain signals. Yoga reduces stress and has action over musculo- skeletal system. Stress itself can act as triggering factor for rheumatoid arthritis.[3]
A 45 year old female with multiple joint pain associated with swelling, morning stiffness, movement restricted and loss of appetite. She was diagnosed with amavata. Treatment includes deepana-pachana with amapachanavati for 1 week. It was followed by internal administration of cow’s ghee in escalating dose pattern for 5 days. Fomentation was done for the next 3 days which was followed by therapeutic purgation (virechana) with Trivritaavaleha (100gm) and castor oil (20ml). After completion of virechana and diet protocol (samsarjana krama), the 40% reduction in pain and stiffness of joints. RA factor was reduced from 94 IU/ml to 50 IU/ml after virechana. The patient was put on specific diet pattern after virechana. After 3 months of treatment, there was significant reduction in all signs and symptoms of amavata. IgE was reduced from 680 kU/L to 53.7 kU/L.[25]
Research updates
A double dummy randomized pilot trail was conducted to compare classic Ayurveda, methotrexate (MTX), and their combination in rheumatoid arthritis (RA) for 36 weeks. Forty-three seropositive RA patients were diagnosed on criteria by American College of Rheumatology (ACR) criteria. The treatment groups included MTX plus Ayurvedic placebo (n = 14), Ayurveda plus MTX placebo (n = 12), or Ayurveda plus MTX (n = 17). It was observed that all three treatments were approximately equivalent in efficacy. Adverse events were numerically fewer in the Ayurveda-only group. [26]
References
- ↑ Basisht GK, Singh RH, Chandola H. Management of rheumatoid arthritis (Aamavata) using symbiohealth healthcare system. AYU [serial online] 2012 [cited 2021 Jul 24];33:466-74. Available from: https://www.ayujournal.org/text.asp?2012/33/4/466/110513
- ↑ 2.0 2.1 2.2 2.3 2.4 Madhavakara. Madhava Nidanam (Roga vinischaya). Translated from Sanskrit by K. R. Srikantha Murthy. 8th ed. Varanasi: Chaukhambha orientalia;2007
- ↑ 3.0 3.1 Mooventhan A, Shetty GB. Effect of integrative naturopathy and yoga in a patient with rheumatoid arthritis associated with type 2 diabetes and hypertension. Ancient Sci Life 2017;36:163-6.
- ↑ 4.0 4.1 4.2 Deshpande SV, Deshpande VS, Potdar SS. Effect of panchakarma and Ayurvedic treatment in postpartum rheumatoid arthritis (amavata): A case study. J Ayurveda Integr Med. 2017 Jan-Mar;8(1):42-44. doi: 10.1016/j.jaim.2016.10.003. Epub 2017 Mar 14. PMID: 28302414; PMCID: PMC5377475.
- ↑ 5.0 5.1 Mahto RR, Dave AR, Shukla VD. A comparative study of Rasona Rasnadi Ghana vati and SimhanadaGuggulu on Amavata with special reference to Rheumatoid arthritis. Ayu. 2011 Jan;32(1):46-54. doi: 10.4103/0974-8520.85724. PMID: 22131757; PMCID: PMC3215416.
- ↑ 6.0 6.1 6.2 Basisht GK, Singh RH, Chandola H. Management of rheumatoid arthritis (Aamavata) using symbiohealth healthcare system. Ayu. 2012 Oct;33(4):466-74. doi: 10.4103/0974-8520.110513. PMID: 23723661; PMCID: PMC3665188.
- ↑ 7.0 7.1 Baria R, Joshi N, Pandya D. Clinical efficacy of Panchamuladi Kaala Basti (enema) in the management of Amavata (Rheumatoid Arthritis). Ayu. 2011 Jan;32(1):90-4. doi: 10.4103/0974-8520.85737. PMID: 22131764; PMCID: PMC3215425.
- ↑ 8.0 8.1 Thanki K, Bhatt N, Shukla VD. Effect of ksharabasti and nirgundighanavati on amavata (rheumatoid arthritis). Ayu. 2012 Jan;33(1):50-3. doi: 10.4103/0974-8520.100310. PMID: 23049184; PMCID: PMC3456864.
- ↑ 9.0 9.1 9.2 Maragalawaththa MG, Goyal M. Efficacy of SeetaramaVati(A Sri Lankan traditional drug) and VatariGugguluin the management of Amavata(rheumatoid arthritis)-an open labeled randomized comparative clinical trial. AYU 2019;40:97-103.
- ↑ Sharma H, Clark C. Diet and digestion. Ayurvedic Healing. 2 nd ed. Philadelphia: Singing Dragon; 2012. p. 71-93.
- ↑ Govinda Das, Bhaishajya Ratnavali, Amavata Chikitsa, 29, Commentary by Ambika Datt Shastri. Reprint ed. Varanasi: Chaukhambha Prakashan; 2012. p. 613-32.
- ↑ 12.0 12.1 12.2 Chakrapanidatta, Cakradatta (Chikitsasangraha). Edited by Priya Vrat Sharma. 3rd ed. Varanasi: Chaukhambha publishers; 2002
- ↑ Soni A, Patel K, Gupta SN. Clinical evaluation of VardhamanaPippaliRasayana in the management of Amavata (Rheumatoid Arthritis). Ayu. 2011 Apr;32(2):177-80. doi: 10.4103/0974-8520.92555. PMID: 22408298; PMCID: PMC3296336.
- ↑ Singh JP, Antiwal M, Vaibhav A, Tripathi JS, Tiwari SK. Clinical efficacy of Rasona Pinda in the management of Amavata (rheumatoid arthritis). Ayu. 2010 Jul;31(3):280-6. doi: 10.4103/0974-8520.77149. PMID: 22131727; PMCID: PMC3221059.
- ↑ Thankamma A. Rheumatoid arthritis and astercantha longifolia. Anc Sci Life. 1999 Jan;18(3-4):247-9. PMID: 22556897; PMCID: PMC3336470.
- ↑ 16.0 16.1 Gokhale B.V. Amavataroga.In: Chikitsapradeep.Pune:Dhanwantary Pratishthan;1989
- ↑ 17.0 17.1 Lekurwale PS, Pandey K, Yadaiah P. Management of Amavata with 'Amrita Ghrita': A clinical study. Ayu. 2010 Oct;31(4):430-5. doi: 10.4103/0974-8520.82033. PMID: 22048534; PMCID: PMC3202259.
- ↑ 18.0 18.1 18.2 18.3 18.4 Edavalath M. Ankylosing spondylitis. J Ayurveda Integr Med. 2010 Jul;1(3):211-4. doi: 10.4103/0975-9476.72619. PMID: 21547050; PMCID: PMC3087367.
- ↑ Pandey SA, Joshi NP, Pandya DM. Clinical efficacy of Shiva Guggulu and SimhanadaGuggulu in Amavata (Rheumatoid Arthritis). Ayu. 2012 Apr;33(2):247-54. doi: 10.4103/0974-8520.105246. PMID: 23559798; PMCID: PMC3611626.
- ↑ Patel SS, Shah PV. Evaluation of anti-inflammatory potential of the multidrug herbomineral formulation in male Wistar rats against rheumatoid arthritis. J Ayurveda Integr Med 2013;4:86-93.
- ↑ Khagram R, Mehta CS, Shukla VD, Dave AR. Clinical effect of Matra Basti and VatariGuggulu in the management of Amavata (rheumatoid arthritis). Ayu. 2010 Jul;31(3):343-50. doi: 10.4103/0974-8520.77167. PMID: 22131737; PMCID: PMC3221069.
- ↑ 22.0 22.1 Sasane P, Saroj UR, Joshi RK. Clinical evaluation of efficacy of Alambushadi Ghana Vatiand Vaitarana Basti in the management of Amavatawith special reference to rheumatoid arthritis. Ayu 2016;37:105-12.
- ↑ Tiwari S K, Singh Jai Prakash. Clinical Evaluation of Alambushadi Compound and its Vasti in the management of Amavata (Rheumatoid Arthritis). Ayu. 2009 Jan;30(1):62-67.
- ↑ Aswathy YS, Anandaraman PV. Therapeutic influence of some dietary articles on gut microbiota in the pathogenesis of rheumatoid arthritis (Amavata) - A review. Ayu. 2019 Jul-Sep;40(3):147-151. doi: 10.4103/ayu.AYU_192_19. Epub 2020 Aug 8. PMID: 33281390; PMCID: PMC7685262.
- ↑ Gupta SK, Thakar AB, Dudhamal TS, Nema A. Management of Amavata(rheumatoid arthritis) with diet and Virechanakarma. Ayu 2015;36:413-5.
- ↑ Furst, Daniel E. MD*; Venkatraman, Manorama M. PhD†; McGann, Mary MPH, MSW**; Manohar, P. Ram MD (Ayurveda)‡; Booth-LaForce, Cathryn PhD†; Sarin, Reshmi MD (Ayurveda)‡; Sekar, P.G. MBBS**✠; Raveendran, K.G. BAM&S‡; Mahapatra, Anita MD§; Gopinath, Jidesh BS‡; Kumar, P.R. Krishna BAM&S‡ Double-Blind, Randomized, Controlled, Pilot Study Comparing Classic Ayurvedic Medicine, Methotrexate, and Their Combination in Rheumatoid Arthritis, Journal of Clinical Rheumatology: June 2011 - Volume 17 - Issue 4 - p 185-192 doi: 10.1097/RHU.0b013e31821c0310